Victor A. McKusick
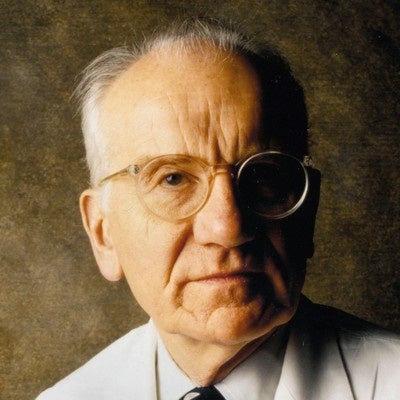
Victor A. McKusick, University Professor of Medical Genetics at Johns Hopkins, is widely considered the founding father of the field. He founded the first medical genetics clinic at Hopkins in 1957, and in the 1960s, launched Mendelian Inheritance in Man, an annually updated catalog of human phenotypes, now published online. His studies of hereditary disorders in the Amish became a model for other studies in genetically isolated population groups. He remained a spokesman of the field throughout his career, contributed his own analyses of its historical development, and was an early advocate for the mapping of the human genome. Dr. McKusick died in July, 2008.
Biographical Sketch
Victor McKusick was born in 1921 in Parkman, Maine. He attended Tufts University in Boston and in 1946 received his M.D. from Johns Hopkins University. He remained at Johns Hopkins for his entire career, becoming an Assistant in Medicine in 1947, in the cardiology unit, rising through promotion to Professor of Medicine in 1960, becoming Professor of Epidemiology in the School of Hygiene and Public Health in 1969, Chairman of the Department of Medicine 1973-85, and University Professor of Medical Genetics in 1985, the title he holds today. In 1957, he was appointed Physician-in-charge of the Joseph Earle Moore Clinic at Hopkins, and established the country’s first Division of Medical Genetics within the Moore Clinic. In addition to this pioneering achievement, Dr. McKusick is probably best known for his pedigree studies of Amish communities and for creating Mendelian Inheritance in Man (MIM), the listing of known human genetic disease markers, originally produced as a mimeographed sheet in 1958, developing into a published catalog based on computerized data in 1966, and appearing in successively more detailed editions before taking its current digital form as OMIM in 1987. Dr. McKusick was the founding editor of Genomics (with Frank Ruddle), the founder-president of the Human Genome Organization, a Member of the NAS Committee on Mapping and Sequencing the Human Genome 1986-88, and Chair of the NAS Committee on DNA Technology in Forensic Science 1990-92. He received the Lasker Award in 1997 and the National Medal of Science in 2002. Dr. McKusick died in July, 2008.
TOPICAL OUTLINE
The interview is organized chronologically, beginning with McKusick’s childhood and youth in Maine; early exposure to medicine and education at Tufts and Johns Hopkins; developing interest and research on heritable disorders of connective tissue (Peutz-Jeghers and Marfan syndromes); founding of the Division of Medical Genetics at Hopkins and organization of the Division; development of the Short Course in Medical Genetics at Bar Harbor; studies of the Amish; origins and development of Mendelian Inheritance in Man (MIM) and OMIM and the impact of these tools on the field; early ideas and efforts to sequence the human genome, culminating in full-scale projects in the 1980s; development of the American Society of Human Genetics and American Board of Medical Genetics. Major topics of interest include developing techniques in genetics and pharmacogenetics; specific advantages of Johns Hopkins as the site for the new specialty; the application of chromosome mapping and linkage analysis to human genetics; funding support for the developing field; the future of medical genetics; and reminiscences of Henry Sigerist, Bentley Glass, Curt Stern, David Price Evans, Malcolm Ferguson-Smith, James Renwick, Frank Ruddle, Craig Venter, and Hamilton Smith.
VICTOR MCKUSICK: A SELECTION OF HIS MAJOR PAPERS
- Jeghers, H., McKusick, V.A. and Katz, K.H.: Generalized intestinal polyposis and melanin spots of the oral mucosa, lips and digits. New Eng. J. Med. 241: 993-1005, 1031-1036, 1949.
- McKusick, V.A.: The cardiovascular aspects of Marfan’s syndrome: a heritable disorder of connective tissue. Circulation 11: 32l-42, 1955.
http://circ.ahajournals.org/cgi/reprint/11/3/321 - McKusick, V.A.: Heritable Disorders of Connective Tissue. St. Louis: C.V. Mosby Co., 1956 (1st edn).
- McKusick, V.A.: Cardiovascular Sound in Health and Disease. Baltimore: Williams & Wilkins, 1958.
- Evans, D.A.P., Manley, K.A. and McKusick, V.A.: Genetic control of isoniazid metabolism in man. Brit. Med. J. 2:485-91, 1960.
- Porter, I.H., Schulze, J. and McKusick, V.A.: Genetical linkage between the loci forglucose-6-phosphate dehydrogenase deficiency and colour-blindness in American Negroes. Ann. Hum. Genet. 26:107-22, 1962.
- McKusick, V.A.: Mendelian Inheritance in Man. Catalogs of Autosomal Dominant, Autosomal Recessive and X-linked Phenotypes. Baltimore: Johns Hopkins University Press, 1966 (1st edn.).
- Donahue, R.P., Bias, W.B., Renwick, J.H. and McKusick, V.A.: Probable assignment of the Duffy blood group locus to chromosome l in man. Proc. Nat. Acad. Sci. 61:949-55, 1968.
http://www.jstor.org/view/00278424/ap000398/00a00270/0 - McKusick, V.A.: On lumpers and splitters, or the nosology of genetic disease. Perspect.Biol. Med. 12:298-312, 1969.
- Gale, A.N., Lacassie, Y., Rogers, J.G., Levin, L.X. and McKusick, V.A.: Two “new” autosomal recessive mental retardation syndromes observed among the Amish. Birth Defects 13(3B): 127-138, 1977.
- McKusick, V.A.: Mendelian Inheritance in Man. Catalogs of Autosomal Dominant, Autosomal Recessive, and X-linked phenotypes. Baltimore: Johns Hopkins University Press, 1986 (7th edn.).
- Hamosh, A., Scott, A.F., Amberger, J., Bocchini, C., Valle, D., and McKusick, V.A. Online Mendelian Inheritance in Man (OMIM), a knowledgebase of human genes and genetic disorders. Nucleic Acids Research 30:52-55, 2002.
http://nar.oxfordjournals.org/cgi/content/abstract/30/1/52 - OMIM: Online Mendelian Inheritance in Man
http://www.ncbi.nlm.nih.gov/sites/entrez?db=omim
1. Early Years in Maine; Childhood Influences; Attending Tufts and Johns Hopkins
ANDREA MAESTREJUAN: It’s December tenth, 2001. I’m Andrea Maestrejuan and I’m with Dr. Victor McKusick and Dr. Anne McKusick for the oral history for the medical genetics project at UCLA. We’ll start at the very beginning, and I’ll ask you, Victor, when and where you were born.
VICTOR MC KUSICK: We were born in Parkman, Maine, on a rather isolated dairy farm on October 21, 1921, so I had my eightieth birthday seven weeks ago [October, 2001]. We went to a one-room schoolhouse for eight years, with the same teacher for seven of those eight years, and then went to the adjoining town to a slightly larger school. There were twenty-eight in our graduating class from high school.
When I say “we,” you probably think I’m using the royal “we,” but I am not. I’m using the appropriate “we” because I’m an identical twin. My twin’s name is Vincent, and my name is Victor, as you know. Vincent ended up in the law and was chief justice of the state supreme court in Maine for fifteen years. I went into medicine, obviously. We split when we went to college, if for no other reason — and there was one reason. Our career goals were different at that time; but the other reason being that we didn’t want to compete with each other for scholarship support, on which we were dependent.
The geneticists are almost more interested in the differences between identical twins than they are in the similarities. An obvious striking difference is the choice of professions between Vincent and me. There’s a good environmental reason for that. I had a long illness when I was fifteen years old and was hospitalized; this is almost impossible to imagine in this day of short hospitalizations – I was hospitalized for ten weeks in the summer of 1937 in the Massachusetts General Hospital. The illness was a microaerophilic streptococcal infection, which began as an abscess in my left axilla, which would not heal, and also involved a large spreading ulcer on my right elbow, with undermining of the edges. It turned out that, as I said, this was a microaerophilic strep, which had not been cultured in Maine because of its unusual cultural characteristics, and I went to two hospitals in Maine before I ended up in the MGH, where it was cultured. Sulfanilamide came in in 1936, and I got sulfanilamide. It [the infection] melted away, healed up, and never came back.
But in the process, I saw a tremendous amount of medicine and a tremendous amount of doctors and decided this was for me. Vincent, who did not have that experience, fortunately, continued his own course. Perhaps I would have ended up a lawyer if it weren’t for the microaerophilic streptococcus. He went to Bates College because of its well-known reputation in the debating field and also because many members of our family, including my father, who was a Phi Beta Kappa graduate of Bates, had attended there.
I went to Tufts because they offered me a full tuition scholarship, and also perhaps the fact that it had a medical school might have had something to do with that. I spent two and a half calendar years at Tufts, three academic years. This was September of 1940 until February of 1943. I took a semester at Tufts in the summer of 1942. Of course, Pearl Harbor occurred in December of 1941.
I went to Johns Hopkins Medical School beginning March 1, 1943. Johns Hopkins Medical School, from the very beginning in 1893, had always insisted on its matriculants having a bachelor’s degree already. This was quite unusual at the time that it was initiated. During the war, however, they let down the bars for a brief time, and I slipped in at that time without a bachelor’s degree. Part of my reverse snobbery is that I was a college dropout, that I don’t have a bachelor’s degree. I have twenty-one [as of June, 2002] honorary doctorates in addition to my M.D., but no bachelor’s degree.
AM: Can I take you back just a little bit?
VM: Yes.
AM: You had posed an interesting counterfactual. You said that if you hadn’t had this experience at Massachusetts General, you probably would have become a lawyer. What was it about law that made it where you might have ended up? And can you think back, maybe in a little bit more detail, what was it about watching all these doctors around you that fascinated you? What was it about medicine and the hospital and doctors that you thought, oh, I want to devote the rest of my life to this? Or was it that simple?
VM: I was being perhaps a little bit facetious in saying that I might have ended up as a lawyer. I think that perhaps there were some more fundamental differences between Vincent and me that would have even directed us in different pathways. I was thinking that I would like to be a minister up until my illness. I don’t know. I’ve never thought too deeply on what fascinated me about medicine, but I don’t think it’s unnatural that I might have been impressed that this was both an exciting and useful thing to do.
There were no doctors in my family, but I saw a lot of GPs in Maine, and specifically, the local GP in Guilford, Maine, who took care of me. I thought he was pretty great. And I guess probably it was a role model sort of thing there. I had full expectations of going back to Maine as a GP when I went to medical school. But in fact, one thing led to another, and when I was ready to go for internship and residency, the most coveted internship, certainly at Hopkins and perhaps anywhere, was the Osler medical internship and residency at the Johns Hopkins Hospital. And I was picked for that, which was very restricted. There were only a few that were picked for that.
Then my boss requested that I be deferred for one more year and stay on as assistant resident. And I stayed on in Baltimore at Johns Hopkins after that uninterruptedly. In fact, I arrived in Baltimore on Washington’s birthday, 1943, to start medical school the first of March. I’d never been south of New York before. Johns Hopkins was the only school I applied for because they announced rather abruptly in the fall of 1942 that they were taking people without a bachelor’s degree, and I jumped at that and got accepted. And I have been at Johns Hopkins, as I say, uninterruptedly since that time.
AM: Before we go on, growing up in this isolated area of Maine, what were the expectations for you in terms of what you and your brother should be doing with your lives from your family, but also in relationship with what the other kids were doing in your school?
VM: Well, we weren’t influenced too much by the other kids. But there were four in the class that finished in this one-room schoolhouse [two in addition to us twins]. The total number of students varied a little bit — twenty-four and twenty six, and so on, in the whole one-room schoolhouse. I’ve always thought that one-room schools had some advantages because you can set the pace at which you proceed because you hear all the recitations and what goes on with all the classes. And you may be involved in teaching some of the younger kids.
My father was a Phi Beta Kappa graduate at Bates and had been a high school principal in Vermont for eight or nine years when he decided he wanted to go back to his home town and do dairy farming. But the academic expectations in our family were very high. Vincent and I were the youngest of five children, and the oldest sister, Grace, had gone to Bates. She was thirteen years older than we and was Phi Beta Kappa at Bates also. Then brother Harry and brother Robert both were high achievers. So we were expected to get out and get an education.
AM: In terms of this unusual kind of step to have this opportunity to go to Johns Hopkins without finishing a bachelor’s degree, how did that influence how things went in your first couple of years at medical school?
VM: I think things went very well in medical school. I should say that, in high school, I took the so-called college prep course. I had no science whatever, no biology, no chemistry, no physics. I had four years of Latin, three years of French, lots of history, lots of literature, and a relatively large amount of mathematics; but none of the other three sciences. When I went to college and took the premed subjects, I didn’t find this overwhelming by any means, but terribly exciting. Biology in particular, I suppose; chemistry and physics were perfectly tolerable. And I think in many ways that I did better in these topics than many of my classmates, who were rather blasé about the whole thing: “Well, I’ve had this before. I don’t need to pay much attention to what’s going on.” But they didn’t represent any problem to me, at any rate.
When I reached medical school, similarly, I didn’t find any problem with deficiencies in preparation. In fact, I was often cited by the people who later at Hopkins experimented with a special program, a so-called five-year program, which took students after two years of college and put them through in three years after that – the so-called five-year program for the combined B.S. and M.D. degree. And some of the people, particularly Dr. Barry Wood, who was an architect of that program, would cite my career as an argument that it isn’t necessary [for all students] to have the prolonged eight-year bachelor/M.D. type program.
AM: Without the kind of high school type courses in biology, after you had this experience at Massachusetts General, how did you feed this interest in biology, or medicine, without taking any courses at high school? Or was that the case?
VM: How did what?
AM: How did you feed your growing interest after your illness? How did you feed your growing interest out there, since there were no biology or chemistry classes to take?
VM: Well, of course, I had a lot of applied biology on the dairy farm. I wrote a little paper at one stage — this was somewhat later — on the coat color inheritance in Jersey cattle. We had purebred Jersey cattle on the dairy farm, some in lines that had been imported from the Isle of Jersey. The Jersey cow is fawn-colored, by and large, but we could show that the fawn color, in fact, is recessive, and there are black Jerseys, and the black is dominant. But, I suppose through the preference of breeders, the fawn color had become dominant. My brother Robert, who was the one who ran the family farm subsequently, and I made this observation in a paper that we wrote up and sent off to the Journal of Heredity and never heard from again. It never got published.
AM: When was this?
VM: I was in medical school by that time.
AM: By this time, you must have had some kind of introduction to genetics.
VM: Yes. Oh, I should say that as far as my interest in genetics is concerned, that really was engendered at Tufts. And as often happens, one can trace that to a very inspiring teacher, a man named Paul A. Warren, who was chairman of the biology department. He was no researcher, but a very inspiring teacher and made genetics so very interesting. I took an elective course in genetics with him, and it appealed to me very much. I can’t tell you exactly why, but it certainly did.
AM: One last thing, to go back, what happened to your interest in the ministry?
VM: That continues, but was put on the sideline as far as a profession. Anne and I are active Presbyterians.
AM: So that aspect of your education never went away.
VM: It never went away, no.
AM: Okay. When you set off for Johns Hopkins to start your medical training, you had this idea that you were going to be a GP and go back to Maine and practice.
VM: Yes.
AM: At what point did this give way to some other alternative career in medicine?
VM: It was a gradual thing. There wasn’t one point in time when I said, well, it’s obvious I’ll never go back to Maine. In fact, when I was eligible to take state board examinations, I took the Maryland boards and the Maine boards at about the same time, in 1947, as I recall. Both of them required that you have an internship.
I graduated from medical school in March of 1946 and interned for a fifteen-month internship from April 1, ’46, until July 1, ’47. I think the summer of 1947, as I recall, as soon as I was eligible, I took both the Maryland boards and the Maine boards because I thought still at that time that there was a possibility, at any rate, that I would be going back to Maine. But I stayed on and on at Hopkins. I was chief resident, which is a pinnacle type of position at Hopkins, exactly fifty years ago now, from 1951 till 1952.
Incidentally, Vincent graduated from Harvard Law School in 1950, and he clerked for Learned Hand on the New York Circuit Court his first year out, and then he clerked for [Felix] Frankfurter on the U.S. Supreme Court in ’51-’52. So I always say that while Vincent was clerking for Frankfurter, I was clerking for Dr. A. M. Harvey, who was my chief at Johns Hopkins. Then I was sort of hooked by that time and stayed on the junior faculty as a cardiologist, interestingly, because there was no such thing as medical genetics. I was involved in founding that later on.
2. Early Work at Johns Hopkins; Marfan and Other Pleiotropic Disorders
I, already at that time, however, had described a new syndrome in my first major paper. It was published in December of 1949 in the New England Journal of Medicine. Actually, it was a very long paper, and they published it in two successive issues, which is a rather remarkable thing to do. But this was based on a patient by the name of Harold Parker, who came to my care in June of 1947, just as I was finishing up my internship. This young man was about fourteen years old at that time and had very striking melanin spots on his lips and inside his mouth on the buccal mucosa. He had a lifelong story of polyps, particularly in the small intestine, which would cause so-called intussusception, when one segment of the bowel telescopes into another segment of the bowel and requires surgery. He’d had several operations for that.
Right after that, another single case came in. Then I had a family in which three members were affected, indicating that it was inherited, and heard by the grapevine that a man named Harold Jeghers in Boston likewise had patients with this syndrome. He had five cases also. So we joined forces in writing these up. Dr. Harold Jeghers came to Washington as the first full-time professor of medicine at Georgetown in 1948, and I would trundle over to Washington and stay with him at his house when we were writing up these cases, which was a very interesting experience. As I say, the paper was published in December of 1949 in the New England Journal of Medicine.
The syndrome of polyps and spots, as we called it, the polyps and spots syndrome — I should say that we were aware, as we noted in our paper, that a Dutchman by the name of Peutz, P-e-u-t-z, had reported this same combination of manifestations in a large Dutch family in the 1920s. In the 1950s, a group at the Mayo Clinic described some of these cases and referred to this condition as the Peutz-Jeghers syndrome, which is what it’s known as now, PJS, Peutz-Jeghers syndrome.
I was responsible for the genetic analysis of that syndrome [in that 1949 paper], because I had access to Bentley Glass here at Hopkins. Glass, after Paul Warren, is the second person who influenced me, and probably even more profoundly than Warren, in genetics. I am really an autodidact as far as genetics is concerned, and the mentoring that I got from Bentley Glass was very important.
In the case of this syndrome, he pointed out to me that this combination of spots on the lips and polyps in the small intestine was not a matter of linkage. It’s very unlikely that there was a gene for spots and a gene for polyps that were linked together on the same chromosome; but that this was much more likely to be so-called pleiotropism, that is, multiple end effects of a single gene, even though we did not know at that time what the reason for the connection might be. And indeed, we do not know with complete clarity to this day the reason for the connection, even though the gene that is mutant in Peutz-Jeghers syndrome has been isolated and specific mutations identified. The physiologic connection still is not completely clear, the pathophysiologic connection.
At any rate, I got training in cardiology because there was no such thing as medical genetics. And I did studies of heart sounds and murmurs, using a method of analyzing heart sounds and murmurs called sound spectrography, which had been developed at the Bell Telephone Laboratories for analyzing speech sounds. In that connection, it was referred to as “visible speech,” for example. But I adapted it to the study of heart sounds and murmurs and did very extensive studies in that way; and in 1958, published a large monograph entitled Cardiovascular Sound in Health and Disease, which used the so-called spectral phonocardiograms for illustration of what murmurs sound like. You could visualize the murmur. This proved to be very valuable for teaching purposes but had no great practicality for diagnostic testing. It had a very interesting application in connection with the category of murmurs that are called musical murmurs. It displayed their harmonics very well.
At any rate, I became known as a cardiologist before I became known as a geneticist, and people often ask, “Why did you switch from cardiology to genetics?” That wasn’t exactly the way it worked because the way it worked was that I was pursuing genetics and cardiology in parallel, and it was more a matter of phasing down cardiology and phasing up genetics.
I told you already about the Peutz-Jeghers syndrome, but in the course of my cardiological experience, I ran up against the Marfan syndrome. Here one had a condition with the patient being unusually tall and gangly, with spinal and anterior chest deformities oftentimes, with defects in the eye, especially dislocation of the lenses, and with a weakness in the media of the aorta, which predisposed to dissecting aneurysm and rupture of the aorta. With my tutelage in the principle of pleiotropism from Bentley Glass, I conceived that this was a syndrome in which one could think of the pleiotropic effects of a single, in this case, autosomal dominant gene, that affected one element of connective tissue, wherever it was in the body.
I collected a large number of Marfan patients and analyzed the families from the pattern of inheritance point of view and analyzed the individual cases from the point of view of the clinical manifestations and natural history of the disorder; and first published on Marfan syndrome in March of 1955 in Circulation, in which I referred to the Marfan syndrome as a heritable disorder of connective tissue, first using that designation.
I looked around for other conditions that might also represent a genetically determined defect of one or another element of connective tissue, wherever it was in the body, and settled on four other conditions. These were Ehlers-Danlos syndrome, osteogenesis imperfecta, pseudoxanthoma elasticum, and Hurler syndrome, the last being the prototype of what we later referred to as the mucopolysaccharidoses. And in 1956, I published a monograph in which the five main chapters related to these five — the Marfan syndrome and the other four related conditions, all pleiotropic disorders.
So my book Heritable Disorders of Connective Tissue actually came out before my Cardiovascular Sound in Health and Disease, which came out in 1958. Heritable Disorders of Connective Tissue went through four subsequent editions, the fifth edition in 1993. The first four editions I did alone as a single author monograph. The fifth edition was a multi-author monograph which was edited by one of my former fellow, Peter Beighton [of Cape Town].
3. Cardiology and Military Service; Anne McKusick
AM: To go back a little bit, what was it about cardiology? Of all the medical specialties a medical student could choose, what was it about cardiology that you wanted to identify with in the absence of, say, genetics as a specialty?
VM: I think that, again, happenstance was involved. As a second year resident in ’47-’48, Dr. Elliott V. Newman, who was in charge of cardiology, asked me to read electrocardiograms. It was quite an honor to be asked to do that, so I was very happy to do that. Then in 1948-50, I worked at the U.S. Marine Hospital here in Baltimore, which had a Hopkins-related unit.
The chief of medicine at that hospital was a man that you know by reputation, Luther L. Terry. He was subsequently Surgeon General, and he was the one who fingered cigarettes as a bad thing. He was a very heavy smoker himself. But he was developing a cardiovascular research unit there, which was due to be transferred to Bethesda as soon as the Clinical Center at the NIH was established. In other words, it was a nucleus for the National Heart Institute.
You should know that I came to Hopkins on a shoestring, really, starting medical school March 1, 1943. The reason I was able to do that is that my brother Robert, who was a bachelor running the firm, lent me money to do it. It was a matter of faith that somehow the money would come on after that. I had been exempt from the draft all this time because I was premed. In the summer of 1943, both the army and the navy set up units at Johns Hopkins. The army unit was called the ASTP, Army Student Training Program. The Navy unit was the V-12. And I was inducted into the service and stationed at Hopkins. The Army paid my tuition and fees, I got a private-first-class salary, and so on. So this was terrific. But what it left me with was an obligation for payback service afterward.
Usually, and for most of my classmates, this caught up with them. When they finished internship, they went into the service. I got a one-year deferment to stay on at Hopkins as an assistant resident. There was only one other person who got that. Then I expected to be going in the first of July 1948; but Luther Terry, who was in the USPHS — the United States Public Health Service runs the marine hospitals, a very old service that goes back to the late 1700s when they were taking care of the Merchant Marines. But they also take care of the Coast Guard, of course. Luther Terry contacted Dr. Harvey, my boss, and asked if he had anyone who could work with him in developing this cardiovascular research unit, and I got the bid for that.
So I transferred from the army to the USPHS and did my two years of payback service in Baltimore. That’s why I say that I’ve been uninterruptedly at Johns Hopkins ever since 1943, because I didn’t even go off for military payback service. Then I came back to Hopkins in 1950 for a year of senior assistant residency. Then I was chief resident in ’51-’52.
You asked why cardiology was appealing to me, and I said that it’s sort of a matter of one thing leading to another. But cardiology certainly is a very respectable and challenging line. I found genetics much more challenging and exciting and novel. As I say, I achieved a reputation in cardiology before [one] in medical genetics. Many people thought that I was committing professional suicide when I cut my links to cardiology and pursued genetics full-time.
AM: I want to pursue just a little bit of a tangent here. When you signed up with the draft to have them pay for your medical education with the expectation that you would have to pay this back, what were your concerns that ultimately you’d end up in a field hospital somewhere in Europe or the Pacific, and that would be the last you were ever heard from again?
VM: I guess I decided to let that take care of itself. That was a matter of concern, certainly; [but there was a war on. It was a matter of signing up with the Army or Navy or not being able to continue deferment. In fact, every able-bodied male did join one or the other unit. The exceptions were persons with health problems or conscientious objectors.]
AM: It was or was not [a concern]?
VM: It was a matter of concern, but it was much better than the alternatives of being drafted out there right off the bat. I think it was the only terms on which I could have stayed out of the active service, on the one hand; and it was certainly the only way I could very easily pay for my medical school education. So what could be better?
AM: And what were the other alternatives for funding medical school after your initial help from your brother?
VM: I think they were limited. I think scholarship support at Hopkins was quite limited for students at that time. Now it’s very abundant, because a big push has been put on that. I know that I discovered when I got here that there were some of my classmates who had scholarship support. They had applied to Hopkins earlier. They’d already graduated, already had bachelor’s degrees.
I sort of got taken on on the spur of the moment. In the fall of ’42, the administration at Hopkins realized they hadn’t filled their class [for March 1, 1943], that everyone was off in the service, and they needed some good people. They of course lowered the bars. But I think the scholarships had been all given out by that time.
There’s an interesting story that’s frequently cited in connection with the need to give scholarship support to students. I went to talk to Dr. [Alan M.] Chesney about whether there was any possibility for scholarship support, and he didn’t have anything to offer to me. Then one day, he called me into his office and there was a gentleman there by the name of Charles Stevenson, who had graduated from Hopkins in 1934. And that Charles Stevenson had been hard-up when he was in medical school, and he’d gone to see Dr. Howard A. Kelly, who was the chief of gynecology and was one of the Big Four doctors of Osler, Halsted, Welch and Kelly. This is the Johns Hopkins medical alumni directory, and this is the famous John Singer Sargent portrait of the four doctors, and this is Kelly back here. Stevenson went to see Kelly.
Incidentally, Stevenson was going into gynecology himself and, in fact, ended up as a professor of OB/Gyn at Wayne State University. But he didn’t have money to pay his tuition, and he asked Dr. Kelly if he could loan him something. Kelly made a loan to him, and Stevenson said, “I’ll certainly pay you back.” And Kelly said, “You don’t have to pay me back. You be sure that you give this to a deserving student in the future.” So Stevenson was just about to go overseas at that time, in 1943, and he handed me a check in the amount of three hundred and forty seven dollars, or whatever it was, that he had gotten from Dr. Kelly.
Dr. Stevenson, when he retired at Wayne State University, went up to New Hampshire and practiced as a country doctor for a while. He’s now in a retirement home well up into his nineties. Anne and I on our way back from Nova Scotia last summer [the summer of 2001] stopped by to see him. A friend of mine did a videotape of the interview between him and me, which I have. It was very interesting to hear his side of the story at that time.
I can’t remember what question started off this discussion, but this gives you an accounting of what would have happened if the army hadn’t come through to pay. I don’t know, although I had explored the possibility of borrowing money. My father had explored that possibility with a local bank in Maine, and I think I could have borrowed money. As it turned out, I never had to borrow money, except from my brother, whom I paid back promptly when I became salaried by Uncle Sam.
AM: I’ll ask you a question now that sometimes this is hard to articulate, and sometimes maybe you can’t articulate it. But you had this experience, at least from the dairy farm, that resulted in a paid —
VM: Could we stop for a minute?
AM: Sure.
[tape off – then resumes]
AM: Okay. Well, we just took a little coffee break. We do have this great opportunity with Anne McKusick here, and you wanted to make a comment about Charles Stevenson. I just want to reiterate that you can jump in any time. I understand that both your work has been collaborative for a very long time, so feel free to jump in and interrupt whenever you want.
ANNE MC KUSICK: I don’t know that I contributed too much on genetics, but I have been part of the support system. (she chuckles)
VM: Part of the support system. Her field is rheumatology, but she goes with me to meetings and, of course, is at home for journal clubs and visiting geneticists, and so on, so she’s very competent in genetics, too.
AMc: I’m interested.
VM: And she’s acquired much knowledge by osmosis.
AMc: The question of scholarship aid for Victor came up earlier, and I was about to bring up the fact that Dr. Charles Stevenson did offer some aid. I think it has been covered already. But that was perhaps your only scholarship aid.
VM: Yes, it was.
AMc: And the fact that you were in the ASTP was your real support through medical school.
AM: Okay. Thanks. And again, don’t even bother hesitating to jump right in. And then when we were drinking our coffee, another memory. We were talking about the history of the science, medicine and technology department at Johns Hopkins, and it’s one of the first and foremost in the country. You were talking about both your experiences with Sigerist. You were mentioning that there was another important reason why you came to Johns Hopkins besides that they allowed people to come in without a bachelor’s degree.
VM: I knew first about Hopkins from a cover story about Henry Sigerist, which was in Time magazine in January of 1939. This was a story about his — this was in the medicine section, and there was a story about his interest in what was called then socialized medicine and was considered on the whole very radical and even communistic by some. The story gave a lot of background on Johns Hopkins, its founding, and especially the founding of the Institute of the History of Medicine at Johns Hopkins, which Henry Sigerist headed up, and the involvement of William H. Welch in that development. I found that very exciting, the entire story; therefore, when I heard about Hopkins again in connection with the possibility of being able to go there, I jumped at it. But I credit Henry Sigerist with having something to do with my being at Hopkins.
And then it was a tremendous privilege when I did get to Hopkins, of seeing a good deal of him. The history of medicine was a required course, and we saw a lot of him, more than might have otherwise have been the case, during the war when the faculty was rather thin. He, for example, was director of the Welch Medical Library in addition to his role as director of the institute because Dr. [Sanford V.] Larkey, the director of the library, was off doing war work. It was he who gave us talks on the use of the library and gave us guided tours.
AMc: My class in medical school was the last class to have the privilege of taking medical history from Dr. Henry Sigerist. We felt that he was a tremendously inspiring teacher and enjoyed his classes. A group of us took him out to dinner and were subsequently entertained at his house and felt that this was a wonderful opportunity to get to know him a little better. He planned to write a six-volume history of medicine, of which I know at least two volumes were completed.
4. The Allure of Books; The Hutchinson Illustrations; The Origins of Medical Genetics at Johns Hopkins
AM: And you had also briefly mentioned the role of the library, the impact of the library and having these resources close by at Hopkins.
VM: As soon as I arrived in Baltimore, there were two institutions that I visited immediately and came to love. One was the Enoch Pratt Free Library, a superb library, particularly at that time, with a magnificent building that was relatively new, and the Welch Medical Library. I found the fact that they had open stacks a novelty compared with what I had known before. The collection of the Institute of the History of Medicine was very rich, and I found that very exciting. But I used to haunt the Welch Medical Library in particular and found that very exciting.
I think that, because of my background, self-education was a necessity. We always did a great deal of reading at home, including reading aloud. But self-education was a necessity, and books have been always very important to me. I head for books as soon as I see them. I remember a fellow intern commenting that, when we had meetings in the department library, that I was always headed for the latest books that had come in, that I was attracted to them.
AMc: Are you going to mention the six trunks in the basement of the Welch Library?
VM: Oh, yes.
AMc: That we spent considerable time going through at one stage.
VM: Yes. I’ve already told you about the polyps and spots syndrome. We discovered that a man by the name of Jonathan Hutchinson, who was an important figure in the history of medicine, a surgeon at the London Hospital, had published for ten years what he called the Archives of Surgery, to which he was essentially the only contributor. He, during his long professional career, which — he was born in 1828, died in 1913. Throughout his busy career, he had an artist continually on his staff, like we might have a photographer, who did water color illustrations of skin lesions, of specimens that he had removed surgically. He did a lot of dermatology because dermatology was considered a branch of surgery at that time. Of course, venereal disease was considered a branch of surgery. And he had this marvelous collection and had a museum of it in his later years. He also ran a clinic on Saturday mornings, at which doctors would bring very strange and puzzling patients to his clinic. And he collected a tremendous amount of this illustrative material. After he died in 1913, William Osler, with money provided by one of the Marburgs here in Baltimore [a wealthy family who made many philanthropic contributions to Hopkins], purchased the collection from his estate and sent it to Hopkins.
I learned when we were studying the polyps and spots syndrome, it was called to our attention by Dr. Chester Keefer in Boston, that Jonathan Hutchinson in his Archives of Surgery had a beautiful color plate of identical twins who had spots on the lips and inside the mouth, a very famous illustration. Obviously, precisely the same type of spotting as in my patient, Harold Parker.
Then we learned that a man named F. [Frederick] Parkes Weber – whose name is known in connection with the Sturge-Weber syndrome and the Klippel-Trenaunay-Weber syndrome – who was in London but always pronounced his name in the Germanic manner because his father, Sir Herman Weber, had come from Germany to England because he wanted to get familiar with Shakespeare in English. He was Queen Victoria’s physician. F. Parkes Weber, in 1919, had done a paper on abnormalities of pigmentation and had referred to these identical twins and stated that one of the twins had died of intussusception at the age of twenty-two, something of this sort.
This, of course, piqued our interest. Through a dermatologic friend at Guy’s Hospital, we were able to trace out the fate of the other twin and found that she had died of breast cancer in her early forties. Breast cancer and other tumors have an increased frequency in the Peutz-Jeghers syndrome, so that may have been significant.
And there was a biography of Jonathan Hutchinson written by his son Herbert Hutchinson, and it gave in there this story that Osler had bought the collection and that it had gone to Hopkins. At that time, in the late forties, I thought — I’d been at Hopkins all of six years, which I thought was a fairly long time. But I had never heard about this, so I inquired from Dr. Chesney, the dean, and he said he thought that the collection was in the Welch Library, and indeed I found that it was there in six large crates, which had arrived apparently about 1914. And covering the top of the crates were large posters advertising British war bonds that had been used as packing. And these were crate after crate of these wonderful water colors.
So I spent a large amount of time for two or three years going through this collection, cataloging it. Based on Hutchinson’s extensive writings and on this collection, I wrote a clinical biography of Hutchinson, which was published in 1952, entitled The Clinical Observations of Jonathan Hutchinson.
AMc: We spent our dates going through things in the crates. (all laugh)
AM: How romantic.
VM: Very romantic, yes. We also had several exhibits of the material.
AM: Okay. Let’s start back then with your development as a geneticist. Up to this point, it seems to me that, without a formal setting to practice genetics, it was basically things that you were presented with, whether it was some observations on your dairy farm or some clinical presentations as an intern and resident, and that cardiology then became a practical identification for you. So, during this time, if a medical student wanted to become interested in genetics and become identified as a geneticist with no structure or institutional forum to take, how did one do this?
VM: One couldn’t. One couldn’t. The one major development occurred July 1, 1957, which made that possible. Medical genetics became institutionalized at Johns Hopkins July 1, 1957, when Dr. Harvey, who was chairman of the department of medicine and my boss, asked me to take over the direction of a clinic that a man named J. Earle Moore had developed as a chronic disease clinic. And this I agreed to do, on the terms that I be permitted to develop a division of medical genetics within the department of medicine, comparable to the division of cardiology, the division of endocrinology, the division of gastroenterology, and all the rest – to do what those divisions do, namely, research, teaching, and patient care, in a particular subspecialty area, arguing that genetic disease is the ultimate chronic disease, since it’s lifelong.
AMc: Wasn’t it even before this, though, that you were following up on families that had the particular disorders?
VM: Oh, yes. I’d indicated that already, that I had done a tremendous number of family studies. I was doing genetic research in parallel with my cardiological research and working up all of this material for the 1956 monograph on heritable disorders of connective tissue. But as far as institutionalization, that occurred when I took over this clinic.
This was a very good arrangement because Dr. Moore already had training grant funds from the NIH, for example, for supporting this chronic disease operation, and I redirected those along genetic lines, which was a very attractive possibility to the NIH. The funds for the program actually were from the National Heart Institute, and I already enjoyed a good reputation with them, and they were recognizing the importance of genetics in heart disease at that time.
With the training grant and research funds, I could take on Fellows, and I could engage colleagues who would develop various areas of medical genetics, including cytogenetics, biochemical genetics, population genetics, and statistical genetics, and so on. I recruited a very large number of Fellows, more of them from abroad, particularly from the U.K., than from this country. It took a little doing to persuade the people in this country that this was an exciting thing to do, although that came along in due course. But I had a large number of fellows from England who were delighted at the opportunity — they came to me as undifferentiated internists or undifferentiated pediatricians. Many of them came early on to work in a chronic disease unit, and I really proselytized them to the field of medical genetics. They came to see that this was an exciting area in which to do clinical work and to do research.
5. The Galton-Garrod Society; Teaming up with the Jackson Laboratory; Mouse Genetics and Human Genetics
AM: So, before the fifties then — well, would you describe yourself then as self-trained in genetics?
VM: Oh, indubitably.
AM: Were you picking up Mendel’s work and reading it, or how did you train yourself to be a geneticist?
VM: Well, I read very extensively in what was available at that time in human genetics. [J. A.] Fraser Roberts in England had a thin monograph on the subject of medical genetics. The most influential textbook, I think, was that of Curt Stern, which was published, I believe, in 1952 in a first edition. That I studied very carefully. But my mentor was, of course, Bentley Glass, as I’ve already mentioned.
A group of us who were interested in medical genetics founded a little society that we called the Galton-Garrod Society. There were three of us in particular: Barton Childs, with whom you’ll be talking; Abe Lilienfeld, who is no longer living, an epidemiologist of great note; and myself. We used to get together and sponsored a series of lectures to which we would invite the people here.
In my educational process, later on — I think a very defining experience was the first World Congress of Human Genetics in Copenhagen in 1956. Have you read my History of Medical Genetics?
AM: There’s a couple of different ones.
VM: This is chapter one in the [Alan] Emery and [David] Rimoin textbook [Principles and Practice of Medical Genetics]. The new edition is about to come out. It has some extensions on it. But I’ve always considered 1956 a watershed year in the history of medical genetics, because that was the year that the human chromosome count was finally gotten right. It’s very remarkable that that was three years after Watson and Crick had deduced the structure of DNA; that the structure of DNA should be worked out before the correct chromosome number was known in the human is a bit amazing. But that’s the way it was.
But the conference in Copenhagen was very exciting. It sort of was a snapshot of the state of the field at that time, which was rather primitive. At that conference, Dr. [Joe Hin] Tjio had an exhibit showing his chromosome spreads, which you had to count as forty-six, without a doubt, in number. But there were lots of other exciting things that went on at that time.
Then my education was continued because — well, the funding that we had from the NIH, I used that to have a visiting professor come for a one-month period and stay with us; and give three lectures a week, on Monday, Wednesday, and Friday at 5:00 p.m. in our major auditorium.
The first of these visitors was Curt Stern, to whom I referred, a wonderful man and one of the old school lecturers. He was a Ph.D. He was in Berlin at the Kaiser Wilhelm Institute and knew all the greats in German genetics. He came to this country and was briefly at Columbia and then went to the University of Rochester, where he spent a long period. He taught a course in human genetics at Rochester and sort of educated himself and collected the literature in preparation for his book [on human genetics].
Then he subsequently ended up at Berkeley, where he ended up his career. And he was at [University of California] Berkeley when he came to us in January of 1959 for the full month. He lived in the hospital. He gave, as I say, lectures on Monday, Wednesday, and Friday for each of four successive weeks. Hurd Hall was always packed, jam-packed, and there were always five or six department chairmen there. He would cover the blackboard with all sorts of things that guided him in his lecture. He didn’t use slides. Sort of a funny little man with a German accent and very gentle.
AMc: Very pleasant.
VM: Yes. We loved him dearly. And with a shirt collar that was too big. I think his wife must have bought his shirts for him, and she didn’t exactly know what size he was. (he chuckles) But very impressive. The professor of obstetrics and always the professor of pediatrics and Dr. Harvey, my boss in medicine, they were all there. This was very exciting. So that was a contribution to my education.
We visited in Bar Harbor, at the Jackson Laboratory in Bar Harbor, Maine, which is a premier mouse genetics laboratory, as you know. Early in 1959, I had an application in to the NIH to support a project to study linkage and do other things in relation to genetic disease. One of the project site visitors was Earl Green, who was director of the Jackson Laboratory in Maine. Earl knew or would have learned from my C.V. that I came from Maine, and he asked if I had ever visited the Jackson Laboratory. He said, “Well, you must come to visit the Jackson Laboratory.”
So the next time on our regular visits to Maine and Nova Scotia, Anne and I visited in Bar Harbor and visited the Greens and Dr. John Fuller, who was the assistant director for training at the Jackson Laboratory. I was impressed with the fact that, at the Jackson Laboratory, they do in mice the same things that we do in human beings at the Moore Clinic of the Johns Hopkins Hospital, namely identify deviant phenotypes and figure out whether they are genetically determined and, if so, how they are inherited. Try to determine what the basic defect is and what can be done to modify the condition, and so on.
At any rate, the Jackson Laboratory had a great powerhouse of expertise in mammalian genetics and, as was very obvious, Bar Harbor was a terrific place to be in July or August. So the idea was to team together — we from Johns Hopkins, by that time, we’d assembled quite a group, not only in our immediate group but in other departments that we had reached out to in the School of Public Health and in the Department of Biology at Homewood [the JH Homewood campus] and in other departments. Why don’t a group of us from Johns Hopkins team up with a group of you from the Jackson Laboratory and guest lecturers from other institutions and put on a two-week course here in medical genetics?
The idea, according to legend, was conceived over lunch at Testa’s Restaurant, which is a well-known establishment on Main Street in Bar Harbor, on a warm July noon between John Fuller and Anne and me, who were there on that occasion. And the idea caught on.
I, at that time, had recently gone on the Medical Advisory Board of the new National Foundation/ March of Dimes. This is the National Foundation for Infantile Paralysis, which had been founded in 1937 by FDR. When the Salk vaccine came in in ’55 or ’56, whenever it was, the National Foundation felt that they should look around for new worlds to conquer, and they decided to go in on birth defects and arthritis. Arthritis got dropped after four or five years. They stuck with birth defects. The vice president for research at the National Foundation was Tom Rivers, and he was a Hopkins graduate, and I had sent him a copy of my book Heritable Disorders of Connective Tissue. At any rate, I think he was instrumental in getting me appointed to the Medical Advisory Board.
When I went to the meeting of the March of Dimes in the fall of 1959, I spoke to Basil O’Connor and to Dr. Rivers about this idea; I think I had written to them before. They bought into this and supported the course from the beginning. The March of Dimes was the sole support of the course for its first twenty-five years, following which the NIH, particularly the National Institute of Child Health and Human Development, came into the picture and has provided the major support since 1984.
The course has been a marvelous educational experience for myself, of course. And I say that probably I learned as much, if not more, than anyone else. The field is moving so rapidly, and many new areas of expertise have come into the picture. Somatic cell genetics came along beginning about 1966 and being very powerfully important in gene mapping. Molecular genetics came along about 1976.
There was a time in odd numbered years beginning in 1967 and running through 1977 when the course, which started out as Short Course in Medical Genetics — the course on the odd-numbered years was a mouse course, and it was called Short Course in Experimental Mammalian Genetics. The folks at the Jackson Laboratory, I think their nose was out of joint just slightly, thinking that they didn’t get a fair opportunity to present their side of the picture. They thought there was a need for a separate course that focused on the mouse exclusively, so that was run on alternate years, given last in ’77.
1979 came up, which by good rights, would have been a mouse course. But 1979 was the twentieth year of the Bar Harbor course, and it was the fiftieth year of the Jackson Laboratory, which had been founded in 1929. It seemed inappropriate not to have a combined course, so the course that year, and ever since, has been called Short Course in Medical and Experimental Mammalian Genetics.
In effect, what had happened was that there was a lot of difference between mouse genetics and human genetics up to that time. But what had happened was that the two fields had converged to a great extent. Molecular genetics had come in; the recombinant DNA era was with us; and those methodologies could be used in both, of course. Somatic cell hybridization between mouse cells and human cells, I thought, was sort of a metaphor for what had happened in the field with fusion of the two fields of genetics; and somatic cell genetics was another methodology used in studying both mouse and human genetics. So the methodologies were so much alike. Human genetics, an observational science previously, was becoming an experimental science now that one had the cellular and molecular methods. So there was no justification for separate courses, and it’s been a very happy marriage since that time.
Transgenic mice came along in the 1980s. Transgenic mice, as a way to put human genes into the mice, or put human mutations into the mouse, to study the effects has been very important. Then with the complete sequencing of the human genome, and now the mouse genome, comparative genomics, is another very important link.
6. Meeting Anne McKusick; Genetic Tools and Methodologies; the Appeal of Johns Hopkins
AM: Okay. I’m going to take you back. We’re shooting ahead here, and before we continue on this course, I wanted to go back. You did mention some dates, and between all this development of genetics as a medical specialty and professional field there was some dating going on concerning trunks, going through old trunks. So why don’t you tell me a little bit about the scientist’s position as a personal being too.
VM: Good idea. Could we shut it off for just a moment?
[tape off – then resumes]
AM: Okay. After this short pause, we were going to start talking about — I wanted to ask you about your developing personal relationship. When did you meet up? Describe that to us.
AMc: Well, I came to medical school in 1946, and I had been working in physics on the Manhattan Project in Oak Ridge, Tennessee. I had known a cousin of Victor’s there who told Victor that I was coming to Hopkins Medical School. So we met when I was entering medical school and he was an intern. We went together from that time on, [and] were married in June of 1949.
AM: How was it for you? Was this a first? How many professional relationships had you had the opportunity to have in medical school? We have this kind of idea that very few women went into medicine until recently, but here’s Johns Hopkins with women coming in as medical students.
VM: Are you asking how many romantic affairs —
AM: No, no, no. Just, was it natural for you to have women in your courses?
VM: Oh, yes. Yes, of course.
AM: So having women as colleagues was —
VM: Yes. That is right. There were seventy-five in our class, and I guess there were nine or ten women in my class.
AMc: There were nineteen women in my class. They went down to twelve. There wasn’t a quota, but they took more women because the men had not yet completed their –
VM: When the men came back from the war, they had to complete their college, and what men were in Anne’s class were older than the usual.
AMc: My class had seventy-two entering, and nineteen were women.
AM: Okay. I guess we’ll talk more about how your professional and personal relationships intertwined over the years, but to continue talking about your development as a geneticist, when did you first cross paths with Bentley Glass?
VM: I sought him out. That’s very easily identified. It would have been in the fall of 1948. I, at that time, was at the U.S. Marine Hospital, which is just across the way from the Homewood campus of Johns Hopkins University, so it was easy to walk across to Bentley’s office. It was that time I was working intensely on this paper that we were preparing on the polyps and spots syndrome, which was published a year later.
AM: Was he teaching courses at this time?
VM: Oh, yes. He was professor of biology. He was primarily a geneticist, but [in] the department at Homewood, the Department of Biology, everyone was a professor of biology. There were no professors of genetics, professors of embryology, and so on. Dr. Willier, who was chairman of the department, was primarily an embryologist. Bentley Glass, who was in the department, was primarily a geneticist.
AM: You just were talking about some of the great new methodologies and tools that present day geneticists have to work with. At the time you were starting to really work with genetics, human medical genetics, what were the tools that you needed to acquire in order to kind of fulfill your research goals?
VM: The tools were limited. I would say that in many ways, statistics or mathematical genetics or population genetics was the basic science, because one did so-called segregation analysis on pedigrees to determine whether the particular trait agreed with the autosomal recessive hypothesis or an autosomal dominant hypothesis. In other words, whether there was support for one or another type of single gene inheritance. One did population genetic studies on the frequency of the particular disorder, made feeble attempts at determining gene frequencies, and even feebler attempts at estimating mutation rates.
And we were just beginning with the methods of linkage analysis. But at the time — the Division of Medical Genetics got started in 1957 — we did not have chromosomology. We did not have cytogenetics as a tool. The first cytogenetics laboratory was set up in the Moore Clinic in February of 1959 by Malcolm Ferguson-Smith, who came to me as a Fellow at that time. This was probably the earliest cytogenetics laboratory in any large general hospital in this country, clinical cytogenetics laboratory.
That technique was very valuable to the development of the field. We used to have many patients referred to us who, in the family, had some genetic disorder. It might have been something that was quite straightforward as a Mendelian disorder and would be sent to us because of the mistaken impression on the part of the clinician that there must be something you could see in the chromosomes, if this was running in the family. We perhaps didn’t discourage that misconception, because we got a lot of patient material. We had many patients self-referred to us. Our program got a lot of notoriety in the lay press and became well known. Self-referral of patients and families probably accounted for more of our clientele than physician referrals, although we got plenty of them too.
There was a great advantage to being situated plunk in the middle of a large general hospital. I found that to be the case when I was collecting cases of Marfan syndrome and formulating the concept of heritable disorders of connective tissue. Because of pleiotropism in many of these conditions, like an elephant being examined by a blind man, the Marfan patients may show up in the Wilmer Eye Clinic because of dislocated lenses; or they may show up in cardiology, pediatric cardiology, for example. They may show up in the orthopedic clinic because of their other problems. The advantages of being a large, what you might call full-service, bank was that I could “beat the bushes” by going through the diagnostic files of all these other departments, and collecting cases and following up on the cases, collecting information from the medical records, and so on.
But the methodology was limited. It was an observational science, and you had to use statistics to analyze what you observed. But then chromosomes came in. We did have biochemical methods, of course. There were quite a number of inborn errors of metabolism in the Garrodian sense, [in] which we at least could find abnormalities in the urine or in the blood that helped define the phenotype. We, of course, were not working down at the DNA level. We were working at a more superficial level.
AMc: Then pharmacogenetics was an interest at one stage.
VM: Yes.
AMc: The Moore Clinic was involved in studying rate of inactivation of INH [ isonicotinic acid hydrazide, or isoniazid], and it was found that patients either were rapid inactivators or they were slow inactivators, and this was an inherited characteristic.
VM: Yes. Pharmacogenetics got started in the Moore Clinic [with the genetics of metabolism of the antituberculosis drug, INH]. Another example that was beginning to be elucidated about the same time was G6PD [glucose 6-phosphate dehydrogenase] deficiency — in the Mediterranean, in particular — this being the basis of favism, when the fava bean precipitates hemolytic anemia in the people who have deficiency of this red cell enzyme.
But one of these Brits who came to me as a fellow in 1958 was David Price Evans, who came from Liverpool. He got the idea from a visiting lecturer who pointed out that the anti-tuberculosis drug, isoniazid, which Anne mentioned, was acetylated rapidly in some people, and in other people much more slowly. This made a difference when you were using it to treat TB, because the rapid acetylators would inactivate the drug and you wouldn’t get full benefit of the treatment. Well, Price Evans, who was, like the rest of us, schooled in the idea that there must be a genetic basis of all sorts of things, thought he would study the basis for this. And he showed in family studies that, indeed, it was inherited, slow inactivation being the recessive condition. This was a pioneer piece of pharmacogenetics.
AMc: At the time, I was studying the shoulder-hand syndrome in patients who were treated with anti-tuberculous drugs, and he showed that a large number of my patients who had developed this syndrome were, indeed, slow inactivators of INH.
AM: I know that Anne needs to leave here pretty quickly, so let me ask one more question before we end for right now. You had mentioned that it was fortunate that Johns Hopkins was located and your work was located in a city that had a large public hospital. But other cities, including Boston, had such a situation too.
What is it about Johns Hopkins that it becomes this center and kind of a proponent for human genetics?
VM: Of course, I’m biased and narrow in my view, but I think that Johns Hopkins is a rather special place in terms of – and I hope still is – but, perhaps, particularly was in the 1950s — a special place in terms of integration between departments. I think there are very few places where you would find so many departments of outstanding quality. For example, the Harriet Lane Home is the pediatrics part of the Johns Hopkins Hospital. The Wilmer Institute is the ophthalmology part of the Johns Hopkins Hospital.
Just to cite those two examples, where in Boston or in Philadelphia or in New York did you find a hospital with a large and outstanding pediatric hospital and an eye hospital as an integral part? In Boston and in Philadelphia, the children’s hospitals were off at a distance from the university hospitals. The eye institutes are quite separate institutions, and even though they may be next door, as in the case of the MGH, one finds that the streets that separate them can be very wide.
[At Johns Hopkins] In terms of the resident staff in these various departments, and in terms of the faculty, they all eat in the same dining room, they walk the same corridors.
AMc: They talk to each other.
VM: The integration is of a degree that you’ll find in very few other places. So this made it possible for genetics to develop, because genetics pervades all aspects of medicine. One doesn’t develop a strong program unless that’s taken into account.
AMc: I think also that the Moore Clinic was a very stimulating place for people to work. We had fifteen fellows from Liverpool.
VM: Over the years.
AMc: In all. We had a number of people coming from various places. They were more or less allowed to go ahead on projects of their own choosing, would you say?
VM: Yes.
AMc: You let them have their own lead a bit in studying things. And there were meetings of the whole clinic that discussed interesting patients. I think there was tremendous excitement generated over inherited disease in the clinic. This really led to some very good work.
VM: We would get fellows who would find their way to us. As I mentioned, undifferentiated internists, undifferentiated pediatricians would be guided into genetics, we proselytized to genetics. But also, we would get orthopedic surgeons, ophthalmologists, neurologists, psychiatrists, people from many different specialties. Dentists. We had quite a number of dentists. We had one veterinarian, Don Patterson, who came to us from the University of Pennsylvania, and he’s been the leader, subsequently, in veterinary genetics, doing in the veterinary field essentially what we did in medical genetics.
[brief conversation regarding stopping the interview – not transcribed]
7. On Heritable Disorders of Connective Tissue; Genetics and Heart Disease; Organizing the Johns Hopkins Division of Medical Genetics; Genetic Mapping
AM: It is December 11, 2001. I’m in the home of Dr. Victor McKusick to continue his oral history interview. I wanted to pick up today with some questions I had from yesterday, and some go back to very early into the interview. You had mentioned that in medical school, you had written an article for the Journal of Heredity and it was rejected. How did this rejection influence how you would approach this whole idea of publications? We live in an era now where it’s publish or perish; but how was it back then to get an article published and also kind of a commitment to a career that would place a lot of importance on being able to successfully publish?
VM: In the first place, it might have been when I was a resident; it might have been during my internship year, conceivably, that I wrote that. But it was very early, at any rate. I always had a big urge to publish, and I don’t think [the early failure] dampened that urge.
AM: Okay. I guess to continue on that track, when you were writing the first edition of Heritable Disorders of Connective Tissue and then later, Mendelian Inheritance in Man, what was your commitment at the time that this was just going to be a solid textbook versus a project that you would continue to issue new editions and continue to update, in fact, become this large encyclopedia project?
VM: Heritable Disorders of Connective Tissue is encyclopedic, in a sense, in the coverage of the particular disorders in that category, but not an encyclopedia in the sense of encompassing all knowledge of genetics. New editions – I guess I thought that was likely to come along because these were ongoing studies. The first edition was in 1956, the second in 1960, the third in 1966, the fourth and last that I did alone was in 1972. And in that sixteen-year period, my studies in the heritable disorders of connective tissue were very intensive, and there was a lot of new information that came along. I could show you these books next door that increase in size progressively. There was clearly a need for new editions to get this integrated information out and up to date.
AM: Then, this may just be always a little footnote in the history of medicine, but how do you account for your name not being put into the Peutz-Jeghers syndrome?
VM: (he chuckles) That’s sort of the roll of the coin, I guess. Peutz deserved credit for his family describing the association, and they felt, I guess, that you could use only one name after that and Jeghers was the name they chose. He was the most senior author on the paper. In fact, he was the first author on the paper [and he had called attention to the polyps-and-spots syndrome in a review on skin pigmentation in the New England Journal of Medicine in 1944 – note added by Dr. McKusick].
AM: Okay. Kind of broader question. You were developing an interest in a specialty in medical genetics coming out after a time of notoriety for genetics. The social eugenic movement in the United States was dying after its high point in the 1920s and 1930s; knowing what we do now about the Nazi atrocities during the Nazi regime and during World War II, eugenics had kind of taken on a certain notoriety. How did this situation influence your decision to make this a specialty in your career?
VM: Not at all, I would say, because medical genetics has as its object helping people through understanding of their inherited problems. The outrageous history of eugenics wasn’t any influence positive or negative as far as I was concerned, I would say unequivocally, quite briefly, and to the point.
AM: And also, on the opposite and more positive way, after World War II, the United States government increased attention to the role of gene mutations, primarily because of nuclear weapons and energy and a lot of what happened during World War II in terms of the development of nuclear power and weapons. How aware were you that there was going to be this whole new support for genetics research?
VM: I was aware, of course, of what was going on in that field, but didn’t see it as a source of support. I think much more real to me was the appreciation of the National Heart Institute and perhaps other institutes, others of the NIHs, in their early days, of the importance of genetics, in heart disease in particular.
We had here at Hopkins a man named E. Cowles Andrus, C-o-w-l-e-s, A-n-d-r-u-s, who was a practicing cardiologist here in town and the senior cardiologist at Hopkins. He was the chairman of the National Advisory Council of the National Heart Institute, probably from early on in its founding. He may not have been the first one, but I even think it’s possible that he was. He was very impressed with the importance of genetics in heart disease, so that guided the interests of the National Heart Institute in supporting research in this area. And they did support a training grant and a program project grant [in the Moore Clinic] from a very early stage. And again I would say that that illustrates the focus on disease and the possibility through genetics, the understanding of genetics, to be able to help.
AM: Okay. One more broad question that hopefully we can move forward with then. These days, we can talk about these categories of basic science versus applied science or bench research and bedside research. The clinician and the scientist. M.D.s versus Ph.D.s and M.D.-Ph.D.’s, all these kinds of categories, including funding mechanisms and translational research, too, is another category we use. But when you were beginning on your professional trajectory, what did this mean? What did these things mean to you? A bench scientist versus a clinician versus somebody who moved in between these two worlds.
VM: I didn’t think very much about it.
The problems presented by hereditary disorders were intellectually tremendously challenging, and that was part of the reason I was interested in them. It was obviously necessary to get at root causes in the terms of biochemical defects and, eventually, DNA defects. This obviously required as much armamentarium as one could muster to bring to bear on the problems.
The way I organized the Division of Medical Genetics was along the following lines: In the first place, a central theme of the division was linkage mapping because, for reasons that I could go into, which aren’t entirely completely clear, I had a great interest in mapping genes on chromosomes, and I felt that this was basic to the elucidation of the problems of hereditary disease. Therefore, I had a chromosome laboratory, a cytogenetics group, necessary, obviously, to study the chromosomes. I had a biochemical genetics group. I had a statistical population genetics group, which was involved, among other things, in linkage analysis. I obviously had a clinical genetics group, which was necessary for describing the phenotypes that one was doing linkage studies on.
I also had an immunogenetics group that did the marker typing. At the time we started out doing linkage studies in the late fifties and early sixties, we had a pitifully small handful of linkage markers to work with. We had blood groups, such as ABO and Rh, and we had a few serum proteins, like haptoglobin. We had the hemoglobin variants which could be used and a few red cell enzyme variants that could be demonstrated by electrophoresis or other methods. The immunogenetics group, which was responsible for the blood group polymorphism studies, was very important to the linkage studies.
So these were the five sections of the Division. Malcolm Ferguson-Smith was in charge of the cytogenetics program at the beginning; later, Dr. [Digamber S.] Borgaonkar. The biochemical genetics group was headed up by Ned Boyer, who was my first Fellow, actually. The statistical genetics and population genetics group was headed up by Tony Murphy. The immunogenetics group was headed up by Wilma Bias, B-i-a-s. And I headed up the clinical genetics group and orchestrated the whole thing.
AM: And why this initial interest in gene mapping?
VM: When I was studying genetics in college, and subsequently, I was impressed with the elegance of the mapping of genes on chromosomes in Drosophila [Drosophila melanogaster; the fruit fly]. The beginning of mapping at least; the identification of various linkage groups in the mouse wasn’t known what chromosome they were on until about 1971 or so. But the genes in the mouse could be lumped into linkage groups. This impressed me as a very elegant and impressive way of getting into genetics. It gave a sense of concreteness and a physical reality to the gene, which otherwise tended to be rather a vague concept, a concept only. And I’ve discussed this with other people who are ardent mappers in the past. There are certain people who are innately very interested in maps, and they like to have maps. I think I’m of that breed, probably. That’s the only way I could understand it.
We were already started on our interest and focus on gene mapping as a primary focus for the division in January of 1959 when I told that you that Curt Stern visited here, and he pointed out that the arrangement of genes on our chromosomes is part of our anatomy and that this cannot help but be important. I have frequently used the anatomic metaphor, most recently in an article in the JAMA of November 14 [2001], which was a genetics and genomics issue. I had an article entitled, “The Anatomy of the Human Genome: a neo-Vesalian basis for medicine in the twenty-first century.”
I trace the elucidation of the anatomy of the human genome, beginning in 1956 with the anatomy of the chromosome at a relatively gross level through the mapping of genes on the chromosomes, and then to the ultimate anatomy, the sequence, with the human genome project and indicate how that knowledge has already paid off and has great promise for this century.
AM: When you saw the kind of elegant work being done in Drosophila and mouse genetics, how did you then plan your strategy to bring these techniques, or this elegance, to human genetics?
VM: In 1955-56, there was a young guy named Newton Morton who was doing his Ph.D. thesis at the University of Wisconsin and worked on methods of linkage analysis. He had papers in the American Journal of Human Genetics in ’55 and ’56 that I found very exciting and stimulating. He and C. A. B. Smith, Cedric Smith, at the Galton Laboratory in London had also been working on the methods for linkage analysis in the human. The first linkage estimation in the human — the linkage between color blindness and hemophilia – was done by J. B. S. Haldane in 1937, working with data that Julia Bell at the Galton Laboratory had collected from the literature. Then J. B. S. Haldane and C. A. B. Smith revised that estimate in the late 1940s. So there were roots of experience with linkage analysis. But I think I found Newton Morton’s work in ’55 and ’56 particularly stimulating.
8. On Using Computers; the Moore Clinic; the Value of Home Visits
I should say that in 1958-59, a man by the name of James Renwick, R-e-n-w-i-c-k [pronounced “Rennick”], came to us in Baltimore. He had, like myself, a burning interest in mapping and had already found the linkage between the nail-patella syndrome and the ABO blood group. And he also had an interest at that time in writing –
[telephone interruption – tape off]
AM: You were talking about —
VM: Jim Renwick, yes. He had a great interest in writing computer programs to do the linkage analysis. He spent one half of each year in Baltimore. The other half he spent in Glasgow at that time. This was very fruitful. I had a computer person by the name of Jane Schulze, and Jane Schulze and Jim Renwick wrote the first computer program for analyzing linkage data. This was done on the mainframe out at Homewood at the Johns Hopkins University campus. A publication came out of that. This was a pioneer effort. Dr. Renwick is no longer living. He died of a brain tumor some years ago.
AM: At the time you were beginning to use computers and programming to solve some of these problems in genetics, what were your expectations of how far machine-based technology would advance the field of medical genetics?
VM: I thought there were great prospects there. My main computer man for about twelve years — perhaps more like fifteen years — was a man named David Bolling. He and I and others in our group went to a number of IBM meetings that were devoted to the applications of computers, and we presented at those meetings what was going on in relation to linkage analysis, for example. I think the expectations were very high but could never have predicted how high they would be.
AM: To go back a little bit. Yesterday you mentioned that initially you had difficulty persuading other people in the medical school to allow this transition of the Moore Clinic into something that would specialize in medical genetics from what it was before. Why did you have this? What were the problems that you encountered initially in trying to get this changed?
VM: Well, we were marvelously well funded externally. For many years, my own salary never cost the institution one red penny because of grant funding. I walked into that when I took over from Dr. J. Earle Moore running it the first of July ’57, because he ran a very well-funded program. So I didn’t pay any attention to them. We went full steam ahead. The institution was delighted to have us aboard. I think they rather quickly recognized the excitement of the area and admired what was going on. But when you have the money, if you don’t have to go on bended knee to request support for this grand idea you have, it’s very easy.
AM: After you had the clinic and the tools for geneticists were beginning to change, I imagine the laboratory space, the bench space, was being filled with all kinds of different machines and people that weren’t normally there or weren’t expected to be there. How did you maintain this — whether it’s financial or political support in the face of these rapid changes, which does not look like a clinician’s responsibility, or territory even.
VM: I think Hopkins is, in general, hospitable to that kind of development. But you touch on what was rather a curious situation in the setup in the Moore Clinic. The chromosome laboratory was set up almost in a closet. And indeed, what had been a john was converted into a darkroom, and so on.
I can tell you a very interesting story. At the Lasker Awards luncheon this past September, one of the awardees was Robert Edwards, Bob Edwards, from Cambridge, who, with Steptoe, a gynecologist, developed in vitro fertilization as a reproductive aid, which of course has been tremendously valuable. He wrote to us in about 1967 and expressed difficulty in getting female eggs to work on. Working with Howard Jones, who then was at Hopkins — Howard Jones is a gynecologist who, after retirement from here — he’s up in his nineties now — went to Norfolk [Virginia] and started a program down there and, I think, that the first test tube baby born in this country was from his program down there. This is a very well-known program down there. So Bob Edwards came to Baltimore and spent some months.
[telephone interruption – tape off]
VM: Well, at any rate, Howard Jones provided him with the human eggs, and he set up a little cubicle down in the front of the Moore Clinic, that was used as a patient examining room but was converted to this use, and worked in the cytogenetics laboratory as far as having a hood and culture facilities, and so on. He was assisted by one of my fellows by the name of Roger Donahue, who achieved subsequent fame by mapping the first gene to an autosome. They used to talk about the little man they had growing down in the front room. But what you say — we made use of what space we had. Space was always at a premium. We converted clinical space when necessary to fit everyone in.
AM: And you generally had no problems from the powers that be to do this, or you just didn’t bother to — you just did it.
VM: We didn’t let them bother us. By and large, we didn’t have any great problems.
AM: Okay. To talk a little bit more about your own work. Yesterday, you mentioned that one of the benefits of working at a large general hospital was that patients would come to you and present symptoms. And some of your earlier work was – concerned people who came in whom you saw. But by the sixties, you had decided, it seems, to go out and find populations to study. How do you account for this transition to become more active in finding –
VM: Along that line, I became aware that if you really want to study human genetics and study families in depth, you cannot set yourself down in the clinic and expect the families to come to you. You identify the problem by the patient who comes to see you in the first place, but if you want to know the family in full, you have to get out and do home visiting and go around the countryside, or wherever is necessary, to visit them. That in the first place. Home visiting, I always found very interesting. You get such a different concept of people when you see them in situ, as it were. In connection with the handicapped patients, patients with muscular dystrophy or patients who are blind or have severe disabilities in some way, you get a much better idea of how they’re coping with that, also how their family accepts the problem, and so on, if you visit them in the home.
But quite aside from that, you have to get out to see whether the family members have a forme fruste of the particular disorder. They say, “No, Uncle Joe, he’s perfectly all right. He doesn’t have anything like this.” And you go visit Uncle Joe and you find that he’s really affected. So your pedigree isn’t worth very much until you have checked out all the details.
Also, as we were doing linkage studies on the family, and you have to have —
[telephone rings – tape off]
VM: Both the affected and the unaffected, you need to have samples on, you need to have marker studies on. You can’t expect unaffected individuals to come to the hospital for that purpose. You won’t get full representation from the family. So home visiting and outreach are very important. Then we got involved with studying the Amish, and it was a marvelous population for genetic study.
9. The Amish Studies; Mendelian Inheritance in Man
AM: You’ve discussed in some of your articles that you became aware of the Amish when other work done in that population was pointed out to you. It may have been an obvious choice to choose them as a population to study, but what were the other alternatives to the Amish in terms of a population to study at that time?
VM: At that time, some of my colleagues, such as Carl Witkop, had been studying a tri-racial isolate in southern Maryland and tri-racial isolates in other areas. These people were known as the we-sorts because we-sorts are different from you-sorts. They are African- Caucasian-American-Indian mixture. There were several such groups around. I went on field trips with him and saw some of the interesting disorders that he had studied, but we were not directly involved ourselves. Clearly, the Amish were head and shoulders above all of these other populations in usefulness for genetics.
AM: When you began your study, what were your expectations?
VM: I thought they had to pay off. As you may know, the reasons I got on to them, the reason they were called to my attention was during committee work as a member of the Advisory Committee for the Johns Hopkins University Press, I had an opportunity to read the manuscript for John Hostetler’s book called Amish Society. I said, “My goodness, this is an ideal population for genetic study” and teamed up with John Hostetler, who is — was, he died within the last year — the world’s leading authority on the Amish and other groups, such as the Hutterites, which is another group of this type.
In the Western world, at least in North America, there weren’t other groups that quite satisfied the criteria for useful genetic studies. I had a post-doctoral fellow from Canada by the name of Claude Laberge, who did a doctoral thesis on the French Canadians. He patterned his studies very much after mine of the Amish studies and pointed out the parallels between the two groups, both being founder populations and having good genealogies and large families and relatively restricted geographic distribution, and all of these characteristics. He has continued those studies in Quebec to this day. His thesis was a very useful piece of work.
AM: What was the impact of your work with the Amish, or the Amish study, on your approach to medical genetics after that? How did this study change the way you thought about where your research needed to go, specifically? But also generally in terms of — and this is a very broad question. You can take it several different directions. This whole idea of we need a map of the human genome.
VM: I don’t know that it modified my thinking in any particular direction. We focused first off on dwarfism because that seemed to be a frequent phenotype in the group. We worked that out, as well as quite a number of other single gene disorders, which were unusually frequent in the population. Then we went on to common disorders of complex genetics, and those have been pursued more, although we started some of those at the beginning. For example, David Rimoin did studies of diabetes in the Amish [as a Fellow with me], and studies of diabetes have been continued to this day by Dr. [A. R.] Shuldiner having been introduced to the Amish by myself. Then studies of cancer. We ourselves did studies of cervical cancer in the Holmes County [Ohio] Amish with interesting results.
AM: Where did the idea come from after you published your Amish studies, beginning in 1963, to create then Mendelian Inheritance in Man?
VM: Well, Mendelian Inheritance in Man was quite an independent venture, quite independent from the Amish studies. It was quite independent from Heritable Disorders of Connective Tissue. It was a separate effort. We had a terrific journal club. We started a journal club in the fall of 1957, in which we tried to be very comprehensive in the reviews of the genetic literature at that time, not only the basic genetics literature, but the literature concerning clinical genetics. I had a large group of Fellows who assisted me in that.
And the journal club was particularly successful, I think, because we had a specific goal, namely, the preparation of an annual review of medical genetics, which came out each year — it’s a quite fat affair; I can show you these — in the Journal of Chronic Diseases. We seized that opportunity to illustrate particular disorders with pictures of patients of our own, or material from patients of our own, our pedigrees, and so on, to illustrate the particular points that were being made in the review. These came out annually for six years running beginning in 1958. Fifty-eight, ’59, and ’60 were combined together in one book, and then the ’61, ’62, and ’63 were combined together in one book.
I stopped doing these, and we stopped doing this after 1963 because I had gotten another idea, namely, the desire to, rather than review each year’s progress and reports, to have a comprehensive compendium of all the information up to a given point. And as it came along in a given year, rather than writing an annual review, add on that information to what was already known. The reason I got that idea was that, in ’60, ’61, ’62, I was writing a monograph which was entitled, On the X Chromosome of Man — pardon the sexism. I had three questions in mind, one of which was, What genetic information is carried by the X-chromosome? As a tentative answer to that question, I collected a list of all the X-linked traits that were known up to that time, a catalog of those, with a little paragraph describing each and references to that. I argued that this list was like a photographic negative from which a positive picture, the genetic constitution of the X chromosome, could be derived. It was that comprehensive cataloging of genes on the X chromosome that I had in mind.
Then the Amish studies came along, and I wanted to collect a comparable catalog of autosomal recessive traits, because in that inbred population, we expected to find even new recessives that had not previously been recognized. And indeed we did. And to know the new ones, we had to know the old ones. Then for sake of completeness and with some trepidation, I assembled an autosomal dominant catalog. Trepidation because there was so much tendency to say that a condition was “autosomal dominant, with incomplete penetrance and variable expressivity,” all of this with hand waving, [but] without too much proof. We created two categories [of entries]. Those in which the particular mode of inheritance seemed to be quite well established, we gave an asterisk to; and those in which it was in limbo still, we left without the asterisk. Of course, this was MIM, this was Mendelian Inheritance in Man.
And the first edition of MIM was published in 1966. The subtitle of Mendelian Inheritance of Man for the first 10 editions was, “Catalogs of Autosomal Dominant, Autosomal Recessive, and X-Linked Phenotypes.” We always had the gene in mind, the gene behind the phenotype, however. We did not wittingly create more than one entry per gene, by and large. [In recent print editions (11th and 12th) , the subtitle has been “A Catalog of Human Genes and Genetic Disorders.” – note added by Dr. McKusick].
MIM went on the computer in early 1964. The print version was a pioneer in computer-based publication. David Bolling, whom I mentioned earlier as my computer man, saw me producing these catalogs and having my secretary update them every month or two. He said, “You ought to put this on the computer” — this was before the days of the word processor — “so you wouldn’t be introducing more errors than you want every time you update it. Furthermore, it will help you make the indices when you get around to publish it.” So throughout its existence, the book has been produced by photo offset or the equivalent thereof [from the computer output].
At first, to produce camera copy, we just used the printout from the computer, and the first three editions were all in upper case because that was the only printer we had. Beginning with the fourth edition, which was in 1975, we used the tapes for automatic typesetting. And if you look at the row of books, it looks as if the fourth edition is smaller than the third edition, but that’s because of the greater economy of space with the conventional type style. The twelfth edition was in three volumes in 1998. We had to go to two volumes in ’92. The ’92 and the ’94 editions were in two volumes. Then we went to three volumes in ’98.
Starting in 1986, ’86 through ’94, every March we would close the computer file and have bound books in hand in July, in time for the Bar Harbor course – four months or less, which one can do with this type of production.
Then in about 1980, Don Merritt, who was head of Medical Genetics at Indiana, went to the National Library of Medicine for a sabbatical. He was working there at the Lister Hill, and some of the people he was working with were trying to develop a system for handling free text. It was a system they were developing that they called IRx for Information Retrieval Experiment. Because one of the people in the project was a hepatologist, they were using hepatitis as a body of knowledge which they would try to get around and use to put into some form in this work. Well, Don Merritt realized this wasn’t as good as genetics would be. He realized, of course, that we already had Mendelian Inheritance in Man, a comprehensive body of genetics knowledge, already on the computer, so he asked me if it would be all right if they used it as a test bed for IRx, which they did in the early 1980s.
I should back up and say that we had it on the computer, and it was on the mainframe out at Homewood. Periodically, we would get from the computer big ledger-like printouts of the whole darn thing. We’d set it up on a counter, and when we had new material to be added, we would leaf through these. (he chuckles) Oh, it was terrible. We had problems with duplication and all sorts of things. Very cumbersome to work with.
10. The Implications of MIM and OMIM on the Discovery of Gene Related Disorders
In 1984, Nina Matheson came to the Welch Medical Library as the director. Nina Matheson had previously worked at the National Library of Medicine and had done a nationwide survey, I think for the AAMC, of the use of computers in medical schools. In that connection, and through her work at the National Library of Medicine, she knew about the IRx project, and she knew about MIM being computerized. Right after she came, she said, “Why don’t you put MIM up online? This will be a tremendous aid to you in the authoring process. Furthermore, there’s no reason not to make it public.” It took some doing over and above what we’d already accomplished, but in the lab she set up, they did that. A man named Dick Lucier worked with her on that. It was her invention calling it OMIM for “online MIM.”
I had it available to me in 1985 as an aid in the authoring process. A tremendous aid it was. The search engine that is provided by IRx is marvelous, and I use it to this day. I was using it yesterday. It’s very facile.
Then in 1987, we went public from the Welch Medical Library, and it was distributed from the Welch Medical Library and from Hopkins up until December of 1995, when the distribution went to the NCBI, National Center for Biotechnology Information. David Lipman is the director of NCBI. David was absolutely delighted to have OMIM, which serves as sort of a hub of his databases. Of course, the marvelous thing is the linkages to other databases, many of which they have right there, and the search through several different databases. I prefer to refer to OMIM as a knowledgebase rather than a database because this implies more intellectual input. Database sounds like all you need is some clerks to put the stuff into the proper pigeon hole. But that is scarcely what’s necessary for authoring and editing on OMIM.
AM: What have been the implications for medical genetics, first with the more limited access of the print version but now the online version of OMIM? What has been the impact do you see on the field?
VM: Well, impact is often measured by use. I think the print version had been very heavily used. It certainly has become an essential source, and did become an essential source after two or three or four editions. It was the place you went when you wanted to look something up. So the impact was very great. But undoubtedly, the online version has had much more impact. It’s used very widely worldwide. Whenever I go to remote places – such as Sardinia or Saudi Arabia, I can think of as two cases in point – the first thing I do when I visit my host is to sit down at his computer and get into Bethesda to see whether what I have left with my people to put up online before I left has gotten up, and also inquire about how extensively they use it and with what facility they are able to get online.
The statistics keep going up all the time. It used to be that OMIM was more free-standing than it is now. It’s sort of built into a menu that I’m really not entirely clear to what extent one can sort out the OMIM usage. But the daily usage is very high. There are several mirror sites around the world so that one doesn’t get — it used to be, for example, one wouldn’t get a full count because Japan, Australia, a couple places in Europe, like Heidelberg and Uppsala, had mirror sites where they would download the whole thing weekly, let us say. And how much secondary use that received, I don’t know. I think its impact has been very high.
We keep a quite good tally on disease-related mutations that are discovered in particular genes, and we’re very — well, let me say in the first place, to back up, we’ve been very obsessive about recording any genes that got mapped to specific chromosomal sites, starting from very early on. Beginning with the 1971 edition, which was the third edition, we’ve had in the front material a listing of all the genes that have been mapped or linkages identified, even though the chromosome carrying the genes might not be known. In the 1971 edition, one page encompassed all of that information. Now the gene map, which is tabular, is presented in the front material and also, incidentally, is online. You can go into that tabular gene map. That goes for many pages, and by many, I mean two hundred and twenty pages, or something, in the front material of MIM.
As I say, we’ve been very obsessive about mapping of genes. Of course, with the human genome project being completed, the whole sequence is there, and we have a pretty good idea up to a point that these, these, and these are genes. We don’t know the function of them, and we know where they map because we know where they are in the sequence, so keeping up that comprehensive map is a lost cause. But we’re still very obsessive about recording the map location of any disease-related gene, and that in itself keeps us plenty busy. And we record a good many other genes for which there is a reasonable amount of information on function, even though it doesn’t have any disease-related phenotypes associated with it as yet.
That’s one thing we’re very obsessive about. A second thing we’re very obsessive about is recording disease-related mutations that turn up in genes. The primary entries in MIM have a six-digit ID number. They represent a little essay describing — oftentimes a very long essay — describing the particular disorder and/or the particular gene that is the heading of the essay.
Then, for about fifteen years now, we have been creating allelic variants – [which] is what I call mutations – and giving them sub-entries, which are numbered with the six digits of the primary number of the entry, followed by .0001 for the first one, and then on down from that. For example, the most frequent mutation in cystic fibrosis in the CFTR genes is a deletion of the amino acid 508, which is phenylalanine, and that’s .0001 under the entry for the CFTR gene, [which has the primary number].
Leena Peltonen at UCLA and I did an article called “Disease Gene Discovery in the Post-Genomic Era” for the February 16 issue of Science this year. It was the same issue that had Craig Venter’s big paper in it and a number of other genomics papers. In preparation for that, I prepared two graphs. One graph was entitled “The Pace of Disease Gene Discovery.” In other words, the discovery of genes that had at least one disease-related mutation associated with it. This I could do very easily by searching — with the IRx search engine, I could search for all of those entries in a given year, and I did this for the twenty years between ’81 and 2000. All of those entries that had a .0001 and the year in them — I guess you could see — because as soon as a mutation was described in a gene, a .0001 entry would be created and the year of report would be the date of discovery — it’s a very interesting graph.
The second graph I did was “The Pace of Molecular Characterization of Specific Disorders.” This was also by year. As of today, the total number of genes that had at least one disease-related mutation is approaching twelve hundred. As of today, the number of separate clinical entities, genetic disorders for which a mutation has been identified — and both estimates include somatic mutations causing cancer, incidentally — is about sixteen hundred and fifty or approaching seventeen hundred, perhaps. The number of disorders that have been characterized is greater than the number of genes that have mutations in them, because some genes have several quite dissimilar phenotypes associated with them. Of course, the hemoglobin gene is a case in point, where mutations can cause sickle cell anemia or beta thalassemia or Heinz body anemia, and so on. There are eight or nine [distinct phenotypes due to mutations in the hemoglobin gene].
[telephone interruption – tape off]
11. Mapping and Sequencing the Human Genome
AM: Okay. We’re going to resume after kind of a brief coffee pause, or a long coffee pause, I should say. You were talking about the implications of MIM and OMIM on the discovery of genes connected to disorders. I don’t know exactly what you were going to say next, so if there is —
VM: I think I’d sort of finished that. I was pointing out two very valuable features [of OMIM]: the cataloging of the mapping information and the cataloging of the mutational information, which are add-ons to the straight description of genes and genetic disorders. The subtitle of the book, of the print version, at the beginning and for the first nine or ten editions, was, “Catalogs of Autosomal Dominant, Autosomal Recessive, and X-Linked Phenotypes.” The subtitle in more recent times [beginning with the 11th edition in 1994] has been, “A Catalog of Human Genes and Genetic Disorders.” Of course, in the 1960s, the only way we had of inferring the existence of a gene — and it was only inference — was by a Mendelizing phenotype.
AM: How does the evolution of MIM and OMIM compare to the evolution of genetics in general, in terms of our basic science typical understanding of how genes work? Because when you first developed the catalog, it was one gene, one disorder approach. What was the interaction between what you were cataloging as you went along and what was happening at the bench? Did they interact together?
VM: They interacted very greatly. I can amplify on the statement I made, that in the 1960s the only way we had of identifying a gene was through Mendelizing phenotype. Then somatic cell hybridization came in as a method for mapping genes. And then genes got mapped, and even though there was no recognized Mendelian disorder related to that gene, it would get an entry in MIM. A case in point is thymidine kinase. The gene for thymidine kinase was mapped on chromosome 17 by the somatic cell hybridization method in 1970 or 1971. It was one of the earliest to be mapped by that method. Even to this day, we don’t know any disorder due to a mutation in that gene. It probably would be lethal anyway if there were mutations, and probably there are mutations. But it got an entry in MIM. So the basic science did influence MIM greatly.
Then when the ability to clone genes came along, as soon as a gene was cloned and sequenced, it could also be mapped by in situ hybridization, for example, directly to the chromosomes. Then it would get an entry, of course, in MIM, again even though no Mendelizing disorder due to mutations in that gene was known.
AM: By the eighties, you become involved in kind of the impetus to create a project that would map the entire genome. How instrumental or not instrumental was this whole project, a very, at least two or three decades, long project of cataloging genes and their disorders, to this larger notion that the genome needed to be mapped and you needed to be a part of it?
VM: I think the cataloging, per se, was not the impetus or an impetus — perhaps an impetus but not the impetus. The gene mapping effort in general was the forerunner. In 1969 — I will give you a reprint of this November 14 JAMA article, which traces the history of the anatomy of the human genome. The usefulness of completely mapping all the genes was something that we had been emphasizing in — I don’t think you have a reprint of it because the reprints have just come out in recent times. This is something that we — are you going to be interviewing Barton Childs at the hospital?
AM: Yes, in his office at the hospital.
VM: Well, my office is on Blalock 10, and Della is my secretary, so come up there. You might like to see the scene of the crime anyway and she’ll give you a reprint, or anything else you want.
A number of people had suggested the usefulness to map all the genes. Haldane, in an overall paper [on human genetics] in 1947, had suggested that that was going to be necessary and desirable. In The Hague in 1969 at a world congress on birth defects, a man named Van Creveld from Amsterdam and I were the chairs of the conference. In the closing talk, I said that a good way to get at the problems of birth defects was to map all the genes. Mapping was just starting at that time, and how I thought that was going to be achieved —
But then in 1973, Frank Ruddle and I started gene mapping workshops. These were annual or biennial workshops in which the aficionados of gene mapping from all over the world got together at various places — we moved around — and collated all the information that had come along since our last meeting and got out a report of that information. These were supported by the March of Dimes, another valuable contribution on their part, I think.
These went on right up until ’90 or ’91, and a lot of the human genome project came from those roots. Frank Ruddle was very high on the idea that, by the year 2000, all the genes would have been mapped. Again, I don’t know how he thought that was going to be done. He said, “By the time I retire,” and he was due to retire in 2000. I don’t know whether he has or not. Perhaps he’s been extended. He’s at Yale, as you know.
In 1980 or ’81, I wrote an article on gene mapping and its usefulness to clinical medicine, and I suggested that by the end of the last vintade of the twentieth century — and I invented “vintade” as a parallel to decade, indicating twenty years — that all the genes would have been mapped by that time and could be mapped and should be mapped.
Facilitated methods of sequencing were introduced in 1977 by Maxim and Gilbert and simultaneously by Sanger. In 1981 the complete mitochondrial genome was sequenced by Sanger’s group, all 16,569 nucleotides. I think that sort of thing emboldened the people to think about sequencing the whole nuclear genome.
The rest of the story is very well known. But it perhaps isn’t often realized that, by 1985 when the human genome project was first formally proposed, that so many genes had been mapped by that time by the relatively arduous methods that had come along up until that time. I have the graph in the reprint, in the JAMA paper, that indicates the growth of gene mapping, and about 700 had been mapped at specific chromosome sites by 1985.
During the period 1985 to 1990, it was discussed, debated, and planned, and debated rather strenuously because many people thought it was a crazy idea, that it really wasn’t science, that it was just brick counting. There was no true biology there. It’s very interesting because this was a different approach to research. It was discovery research, and research in biology had been essentially all hypothesis driven before. This was more like astronomical research in a way, and this required a different mental set.
I was on, and Dan[iel] Nathans from here was on, the National Academy of Sciences committee on mapping and sequencing the human genome. This was commissioned in late 1986 and reported out in February of ’88 and came to the conclusion that the project could be done and should be done. They estimated that it could be done in fifteen years, that it could be done for 200 million a year in add-on funding. That figured out to three billion dollars total for the 15-year project, and people found that absolutely mind boggling, such a terribly expensive project. Of course, three billion dollars compares with — the annual budget of the NIH now is over twenty billion. Even the AIDS budget, I think, approaches three billion. Of course, the 200 million a year was in 1988 dollars.
Wally Gilbert was on that committee also. There was a discussion at that time — and it seemed a little bit silly that one would have talked about it, but I guess it was worth talking about — whether one had to sequence the whole thing. Why not sequence just the functional part, just sequence the genes? And Wally Gilbert pointed out, very wisely, I think, that you’re going to have to sequence the whole thing just to find the genes, and that is certainly true.
The committee recommended that one should map first, sequence later. Essentially, they recommended a top-down approach, which is what the publicly funded NIH/DOE program pursued, namely, create genetic maps of DNA markers spaced all along the chromosomes, which could be used as linkage markers, and so on. Then create physical maps, taking the chromosomes apart in overlapping segments. And then do the final map, the sequencing. In other words, a top-down approach.
Then Craig Venter entered the scene, and his first contribution was the development of ESTs [expressed sequence tags], which was very important – which was going directly where the action is, namely the genes, by creating complementary cDNAs by reverse transcriptase from the mRNA [messenger RNA] in different tissues and at different stages of development. He started out at the NIH and was interested in the brain and interested in what genes are functional in the brain, and that is the tissue from which he got the messenger that he did reverse transcription on to create expressed sequence tags, which are little snippets of genes. This was a valuable approach in its own way.
The National Academy of Sciences committee recommended that model organisms should be studied in parallel with the human. I’ve often said that I think this is one of the most interesting — the most interesting, perhaps — and arguably one of the most contributory parts of the human genome project has been the non-human genome projects, because, by the old principle of comparative anatomy — and here is the anatomical metaphor again — one learns so much about the human genome by studying the homologous structures in other genomes.
The first free-living organism for which the genome was completely sequenced was Haemophilus influenzae. This was reported in July of ’95 by Craig Venter and Ham[ilton] Smith [and their colleagues]. Of course, viruses had been completely sequenced before, but no free-living organism. And they used a bottom-up approach. They took the whole circular chromosome of the bacterium and split it up into segments by shearing the DNA and then sequenced the heck out of it by the equivalent of five, six — I don’t know how many times sequencing in toto and then reorganizing it by recognizing overlapping ends of the segments.
I asked Ham Smith one time how he and Craig got hooked up. They were at a meeting together in Spain and chatting, and Ham asked Craig, “Where are your horns?” Craig had a very bad reputation that he was going to patent the whole genome, and he was science’s bad boy, and so on. But they hit it off. Of course, Ham Smith’s pet for several decades had been H. influenzae. It was H. influenzae in which he discovered restriction enzymes first. Hinf is the name of one of the restriction enzymes, which is named for H. influenzae, which he discovered and got the Nobel Prize for. So it was a natural for him to use that. A very creative person, and it was a wonderful synergism.
That was ’95 and, of course, between ’95 and the next four years, they completely sequenced all — “they” being the group at TIGR, which stands for The Institute for Genomic Research — sequenced all kinds of organisms, including very important ones, like one strain of the TB organism; Helicobacter pylori, which causes gastric ulcer; and so on and so forth. And including archeobacteria, which was – from a basic biological understanding, was very important because that seems to represent a third kingdom.
Then they took on Drosophila with the help of the Drosophila community, and finally the human genome.
12. Planning and Evaluating the Human Genome Project; On the Evolution and Future of Genetic Medicine
AM: When you worked on the National Academy of Sciences committee, and being a participant in the decision to go ahead with the human genome project, and you become the founding president of the Human Genome Organization [HUGO], how did you envision your role at this point in the project? As a crisis mediator between the critics who thought this couldn’t be done and the participants who were under tremendous pressure to see this succeed? How did you see yourself standing in between these — as a representative of one side over the other?
VM: I don’t think I saw myself as a crisis mediator.
[telephone interruption – tape off]
AM: We were talking about your own personal expectations for the human genome project. How were you preparing to address critics within the scientific community and within other communities outside of the scientific community?
VM: I was very enthusiastic about its potential and just kept pounding away at that. I think the criticism gradually faded away as the enthusiasm caught on in general. I think people saw it as a very exciting, and for biology, up to that time, a unique undertaking.
AM: We now know the ending to the story, mostly anyway. But in terms of the debates over the timelines, how quickly or how slowly it would be able to proceed, where were you in these debates? And the expectations that, okay, are we going to meet this timeline?
VM: Well, as a member of the committee that set the timelines, they seemed reasonable to me. I think it was recognized that technologic development was going to determine the speed to a considerable extent. And one of the nine or ten major recommendations was that a lot of effort be put into the technology at the beginning.
When the human genome project was formally proposed in 1985, YACS, the use of yeast artificial chromosomes as a means of large segment cloning, had not yet been invented. They were invented in 1987. PCR, which has been so fundamental, was just barely coming in at the end of 1985; and really had its debut at Cold Spring Harbor at a meeting in 1986, at the same time, incidentally, that the human genome project was discussed extensively in a rump session.
The rump session was chaired by Wally Gilbert and Paul Berg, and Jim Watson was sort of restlessly roaming around up on the side of the auditorium. He said, “Why should the DOE get involved in this in addition to the NIH? Why not just the NIH?” And Wally Gilbert said, “Well, one reason is so that we’ll get more money for the project. If you do it that way, you’ll get more total money for the project.”
AM: And Watson’s concerns with participation from the DOE were because? Why did he question their participation?
VM: I guess he thought that better science would be done if it was under the direction of the NIH, that the NIH had a track record of high quality science, and he wasn’t certain the DOE had what it took to undertake a biological problem of this nature. I think that was probably his thinking.
AM: And how did you feel about this joint funding effort clearly between two —
VM: I thought it was okay. The DOE had actually come up with the idea first. They, of course, had responsibility for radiation effects, as you mentioned earlier. They had come up with the idea first at a DOE meeting. They wanted to identify mutations and measure mutation rates, and so on, and they said that since mutations are changes in the DNA, then best we ought to know what the normal sequence is.
AM: In what ways has the human genome project exceeded your even wildest expectations, and in what ways has it maybe fallen short?
VM: Well, it certainly has exceeded my expectations as far as the rate at which it was completed. As I told you, I was making these rash predictions that by the end of the twentieth century, all the genes would be mapped. Well, that was really what was achieved. They were all mapped by sequencing the whole thing. So I guess I could claim that that was an expectation that was fulfilled, perhaps actually exceeded. I don’t think that I have been disappointed by anything that would come out at this stage.
AM: What about the total number of genes in the genome? Clearly, that has caught some people by surprise. How about your own expectations? Where did those fit in?
VM: Yes. I thought that there were more, although I’ve been making estimates of about seventy thousand, that a lot of people thought impossible that there could be as few as seventy thousand. It probably is more than the 38,000 or 40,000 that are talked about. And it might be up to 50,000 or 55,000.
But I think that when you think about it, this makes sense that there are all sorts of mechanisms by which complexity can be achieved in the human, with a number of genes that isn’t all that much greater than the worm or the fly has, with alternative splicing and with post-translational modifications and all such things as this. I find it very credible that, even though we have only 50,000 genes, that we could have 500,000 proteins created off those.
AM: And I’ll ask you to predict the future and where do you see medical genetics going, now that we know the genome and the number of genes in the human genome? Where do you see the science of human and medical genetics moving?
VM: Well, I think medical genetics is moving into genetic medicine. As you know, our institute here is called Institute of Genetic Medicine rather than Institute of Medical Genetics. I didn’t have anything to do with the choice of that title, certainly not with the eponym, but I think “genetic medicine” is very good because genetics pervades all of medicine. When you say medical genetics, it conjures up images of all of these individually rare single gene disorders, [that] in the aggregate represent a large body of disease. When you say genetic medicine, it tells it the way it is, namely, that it involves all of medicine.
That is where medical genetics is going, to a better comprehension of susceptibility genes and the involvement of genetic factors in common disorders, complex traits as they’re called these days, what we used to call multifactorial disorders. I think the medical geneticist will spend much more time overseeing gene screens, or genome screens, interpreting the results to individuals, and designing programs to make the most of the strong points of the genome and to avoid troubles from some of the weak points in the genome.
AM: In one of your publications, you defined human genetics into five periods of time. From 1882 to 1956 as the gestational period. Then there was the golden age. For a few years, there was the doldrums. And then the banding era. And then from ’77 on, the era of molecular genetics.
VM: Molecular cytogenetics.
AM: Cytogenetics. Do you see this categorization changing further still?
VM: That’s just in cytogenetics. No. I think — that’s just in the field of chromosomology, as you might call it.
AM: Okay. Before I ask you some more broader questions about the field of medical genetics, I want to go back a little bit to talk about the creation of a specialty of medical genetics. Before I do, I want to ask a question about — In 1949, the American Society of Human Genetics was created. Most of the members, were Ph.D.s and not so many M.D.s. How did you see yourself fitting in this world of Ph.D.s when you just — just, in quotes — had an M.D.? Was there these categorizations of who to do what in what situations?
VM: I think the field of human genetics at that time was so amorphous, shall we say? Was so ill-formed that it was up for grabs that whoever was interested in it and had confidence in it could join the society and could legitimately consider himself working in human genetics. The M.D.s joined the society because they had interest in some particular disorder; usually they might be ophthalmologists like Harold Falls at Michigan, or they might be orthopedists, rheumatologists, cardiologists, like myself. They had particular disorders that they were studying in depth and had something to contribute and, as in all societies, were seeking kindred spirits that they could share their experiences and insight with. But the field was being defined at the time, and the Ph.D.s worked shoulder-to-shoulder. I don’t think either looked down on the other.
The methodologies were limited. The information that came from other organisms, the experimental organisms, was very valuable in passing over to the observational data on the human. But we didn’t have very much to work with, and in many ways, the physician, with his abilities to define the phenotype, had the tools that were necessary for studying human genetics.
AM: So this whole idea now that we talk about, translational research, really defines genetics from the very beginning.
VM: Yes.
AM: It’s clear from sitting here that you have been a very self-motivated individual throughout your entire life and that you carved out this specialty over the course of your career. Before there was the institutional support, before, say, the late fifties and then before the creation of the boards in the early eighties, how did you attract and motivate students to take the extra step that they would need to take in order to become good geneticists, well-trained geneticists?
VM: I think they were just fired up with interest for the field. It was a field of medicine that was intellectually challenging. It was a field that one could push back the frontiers on. So it was a matter of inspiring people. There was a large interest as far as preparing people for the field, inspiring them to get the necessary training. It can be pointed out that during the 1960s and ’70s, there was a big interest in increasing the teaching of medical genetics in medical schools, an increased recognition of the necessity to increase that teaching, and also there was a recognition that it had some practical clinical utility, especially in connection with the chromosomology that was now possible, in connection with biochemical testing of various types. Prenatal diagnosis by amniocentesis came in in 1966, or thereabouts. All of these things meant that, in the last instance, the departments of OB/Gyn wanted to have genetics in the faculty representation. Departments of Pediatrics were very strong on developing genetics programs. Incidentally, I came from a background of internal medicine, but always, in the Moore Clinic, we saw patients of all age groups.
13. The American Board of Medical Genetics; On Serendipity and Opportunism
AM: Okay. You were talking about how to motivate students to become involved in medical genetics.
VM: I think the motivation was by infectious excitement about the field. As far as the formalization of the American Board of Medical Genetics, I had thought in the 1970s when this question came up that there was no need for such a board.
[telephone interruption – tape off]
VM: I think I was president of the American Society of Human Genetics in 1974, something of that sort. My presidential address was on the development of human genetics as a clinical discipline. I said in there that I thought there was no need for a Board because medical genetics was institution-based, mainly academic institution-based, and that such institutions had ways of regulating the sub-specialists working in them, and there was no necessity for Boards. I was referring to the fact that there aren’t practitioners out in the community that one had to regulate.
I came to that view by talking to a surgeon in Cleveland who was president of the American Boards at that time. He was comparing genetics to the field of nutritionists. They are also institution-based. I sort of swallowed that hook, line, and sinker, I think. [But of course, in fact, both geneticists and nutritionists function outside institutions.]
David Rimoin was a prime mover, in 1981, I think, in developing the American Board of Medical Genetics under the American Society of Human Genetics. It wasn’t blessed by the AMA at the beginning. I was involved with that and took the exams. I refused to be grandfathered into it. So all the Board members did take the exams. We thought it was inappropriate not to do so.
Then the American Board of Medical Genetics, as I recall, became an official member of the family of Boards in ’91, and that really seemed like the thing to do. The American College of Medical Genetics was formed soon after that. I think we were the twenty-fourth member of the family of Certifying Boards, so we had all the appurtenances, just the same as there is an American College of Surgeons and an American Board of Surgery. We’re right in there with all the rest. And it’s really necessary now. And this is because there are so many more things that we can do. Our training has to be up to snuff, and we have to be regulated to whether we perform properly.
AM: Yesterday you spoke about this at the end of our session and spoke about it a little bit today. The one reason why Johns Hopkins came to the fore in medical genetics is because of this interesting institutional form that it had taken where it was drawing from all these different departments and coordinating and integrating very well together. How did having, then, suddenly some kind of structure to put people in, to bring together and then separate them from other departments? Did this work well for the field, or has it been detrimental in some aspects?
VM: You touch on an issue about the question of creating a separate department of medical genetics in this institution, or call it what you will. Creating a separate institute, does this help or does this hurt? This has been a troubling question right along. The Institute of Medical Genetics here is not yet a separate department. It functions directly under the dean’s office. It has many of the prerogatives of a separate department in terms of having the power of appointment, and such like. The chief of the institute sits on the Advisory Board, which is the governing council of the medical school, as a voting member. And sometime it may become a separate department. It has people who have joint appointments in other departments, even appointments in other departments which may be their primary appointment. But I think that it does not destroy the collegiality and the interaction that we’ve enjoyed all along.
In an institution like that as it has developed now, the — cardiology, for example. This perhaps may not be too relevant to this discussion. But the pediatric cardiologists, the adult cardiologists, the cardiovascular surgeons, the cardiovascular radiologists, they have much more to do with each other even though they’re in separate departments, than they do in each case with the endocrinologists or the gastroenterologists, or this or that. It’s sort of like you have a matrix with these departments like this and then various specialty interests that cut across all the departments.
AM: Looking back, now that there is an American Board of Medical Genetics, and you were hesitant at one point in your life to support, what do you think the impact has been on the field by creating a board and a subspecialty?
VM: I think it’s been very favorable and certainly very necessary.
AM: I think that pretty much covers all the questions I had. So I’ll turn it back over to you to address any questions or issues that we haven’t talked about in these four hours. It’s been about four hours of interview.
VM: I think it’s been very thoroughly covered, and I’ve enjoyed talking about it.
AM: I was looking over my notes. If I can insert one last question. Has medical genetics been a field that has moved — in relating your life during this interview, it seems like it was never clear that you were going to be a medical geneticist. That’s not what you started out to be, but somehow your work and your interest developed in that way. The field also. We can make these parallels between your life and the field in a general sense. How would you ascribe agency to that? Was it something just inevitable about it, or was serendipity involved?
VM: I think that — yes. I’ve said several times that when I review my career, it sounds like the confessions of an opportunist, a chauvinist, and a dilettante. Opportunism, you know, is given a bum rap in the dictionary, which defines it as taking advantage of circumstances often without attention to the consequences to others. Opportunism and serendipity are very closely allied, but opportunism is very important in all research, certainly in clinical research. The observations that you make on patients stimulate ideas for research. And I think that that patient, Harold Parker, was a good example of seizing an opportunity — the studies of the Amish were, in essence, an instance of opportunism, when I first learned about the existence of the group and the marvelous characteristics for genetic study, as indicated in John Hostetler’s monograph.
I confess to the sins of chauvinism, parochialism, provincialism, because I’ve been at Johns Hopkins uninterruptedly for a very long time, now going on fifty-nine years since I came here as a medical student. But Hopkins is sort of at the crossroads, both literally and figuratively, and has great breadth and depth so that one could stay here and develop and explore many different areas of research without getting stale, stultified. I never found any need of taking a sabbatical, which I never did take.
As far as dilettantism is concerned, one might consider that dilettantish when you delineate clinical syndromes, when you study the physics of heart sounds and write a book on that, when you do gene mapping, when you study the dynamics of genes in population groups such as the Amish, and so on. I feel very privileged to have had a very large number of very exciting areas of research in which to work. There’s a very famous quote from Isaac Newton. Of course, to compare my career with that of Isaac Newton is absurd, but he says that he feels like a small boy playing on the beach and picking up an occasional pebble that is smoother and brighter in color than the rest while all the great mysteries of the ocean go unexplored. He’s just picking up a little stone here and there. So I feel like an unabashed dilettante, as well as a chauvinist and opportunist.
AM: Well, if there isn’t anything else you’d like to add, we’re — Well, thank you very much.
VM: You’re certainly very welcome. I’ll be around on Thursday if you have any other questions that you want to fill in.
AM: Okay. Thanks a lot.
VM: You’re very welcome.
END OF INTERVIEW